Introduction – Balancing Beauty Benefits with Rare But Serious Risks
Dermal fillers have become a cornerstone of modern cosmetic treatments, offering a non-surgical solution for facial rejuvenation and contouring. While popular for their quick results and minimal recovery time, these treatments carry rare yet severe risks that deserve attention. Beyond common side effects such as bruising and swelling, the possibility of vision loss, although extremely rare, warrants awareness. This article examines the causes, prevention, and management of this devastating complication, providing an essential guide for both practitioners and patients.

The Rise of Dermal Fillers
Dermal fillers are celebrated for their versatility, from lip augmentation to facial reshaping. They are marketed as quick, low-risk procedures with little downtime. This convenience has driven their global popularity, with procedures skyrocketing by 300% between 2000 and 2017. However, their accessibility underscores the need for greater education about risks – particularly blindness, the most feared outcome.
Why Awareness Matters
Though catastrophic complications from dermal fillers are rare, blindness after dermal fillers is life-altering. This article will focus on evidence-based insights to ensure safer practices and informed decisions for anyone exploring filler treatments.
The Mechanism of blindness after dermal fillers
The cause of filler-induced blindness is closely connected to the intricate and fragile blood vessels in the face. The main issue arises when dermal filler is mistakenly injected into a blood vessel. If the filler enters a blood vessel, especially with excessive force, it can move against the normal blood flow. This filler material, made of the substance itself, can then move and block arteries far away, significantly affecting the ophthalmic artery, the main artery providing blood to the eye [2, 3].
The ophthalmic artery, derived from the internal carotid artery, is the exclusive supplier of blood to the retina. When there is a blockage in this artery or its offshoots, such as the central retinal artery, the retina is deprived of oxygen and essential nutrients, resulting in ischaemia. In the worst-case scenario, this can lead to retinal artery occlusion, setting off a series of events that culminate in permanent vision loss [4]. The retina, which is highly metabolically active, can only endure a limited period of ischaemia, with research indicating that irreversible damage can occur in as little as 90 minutes, and some studies suggesting even shorter durations of 12-15 minutes for complete central retinal artery occlusion to result in retinal infarction [5, 6]. This narrow timeframe emphasises the crucial need for immediate identification and intervention in cases where filler-induced blindness is suspected.
The physics of retrograde flow and embolisation play a crucial role. The pressure exerted during filler injection, if it exceeds the systolic arterial pressure, facilitates the backwards flow of the filler material. This is particularly relevant in areas with rich vascular anastomoses, where pathways exist for emboli to travel against the direction of blood flow. The embolic material then lodges in smaller arteries, causing occlusion and disrupting blood supply. Understanding this mechanism is paramount for practitioners to appreciate the inherent risks and implement meticulous injection techniques to minimise the likelihood of intravascular events.
Safety of Hyaluronic Acid Fillers
Assuming that hyaluronic acid (HA) fillers are completely safe because of the presence of hyaluronidase, an enzyme that can break down HA, is a dangerous misconception. While hyaluronidase is useful for managing complications from HA fillers, it does not remove the risk of blindness.
The widespread use of HA fillers, accounting for approximately 80% of the dermal filler market, contributes to their higher representation in reported cases of blindness [7]. However, it is imperative to recognise that all injectable fillers, regardless of their composition, carry the potential for intravascular injection and subsequent vascular occlusion. Furthermore, while hyaluronidase can theoretically dissolve HA emboli, its effectiveness in reversing blindness is limited by several factors, including the time elapsed since the occlusion, the accessibility of the hyaluronidase to the embolus, and the extent of ischaemic damage already sustained.
The physical properties of HA fillers, such as viscosity and degree of cross-linking, also influence the risk profile. Fillers with higher viscosity and greater cross-linking may be more prone to causing severe vascular occlusions due to their cohesive nature and potential to form larger, more obstructive emboli. These factors highlight that while hyaluronidase offers a crucial management tool for HA fillers, it does not negate the need for meticulous technique and preventative measures to avoid intravascular injection in the first instance.
High-Risk Facial Zones
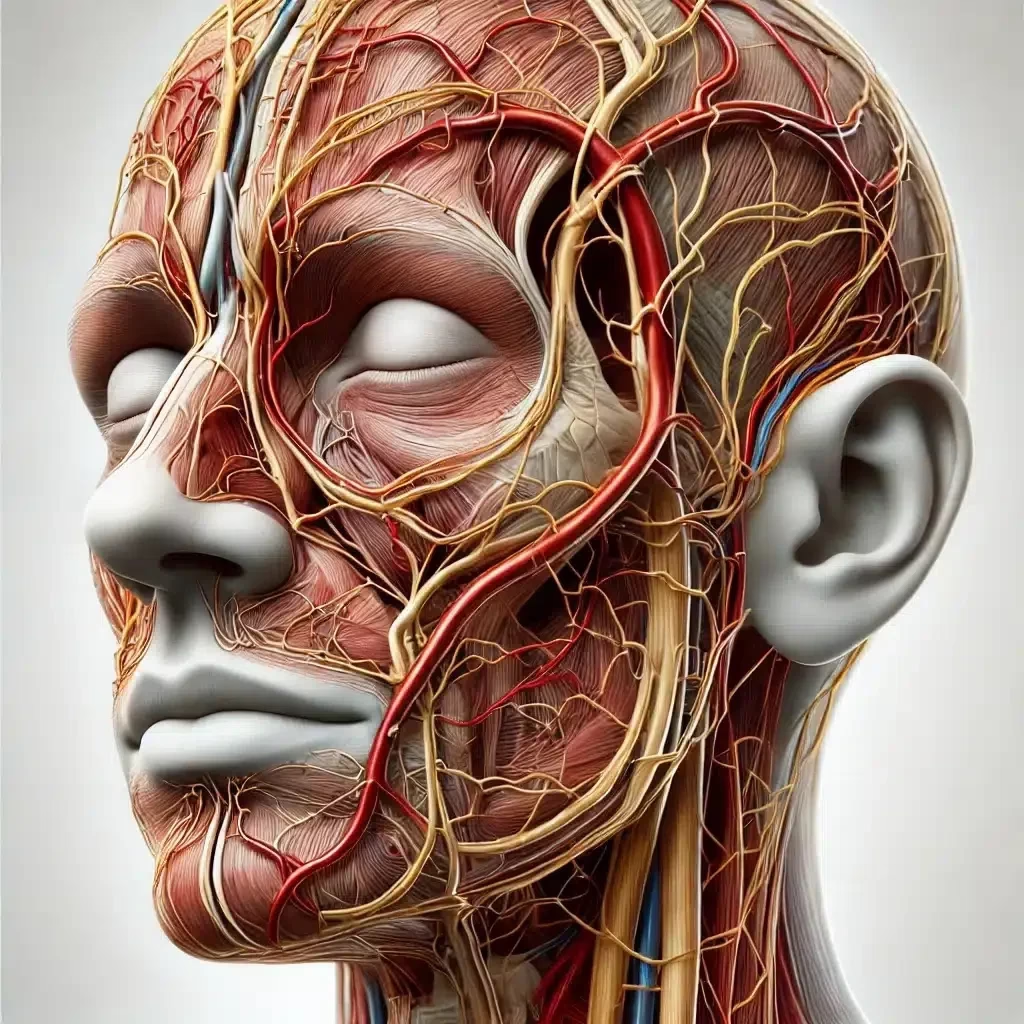
Certain facial regions are anatomically predisposed to a higher risk of vascular injection and subsequent blindness due to their intricate and interconnected arterial networks. These “high-risk zones” demand utmost caution, meticulous technique, and a deep understanding of facial vascular topography. These areas include:
- Nose: The nose, particularly the nasal dorsum and tip, is considered the highest-risk area. Its rich vascular network, with arteries like the dorsal nasal artery, lateral nasal artery, and alar nasal artery, and their proximity to the ophthalmic artery via anastomoses, makes it particularly vulnerable to embolic events [8, 9]. Procedures like non-surgical rhinoplasty, which aims to reshape the nose with fillers, carry a heightened risk.
- Glabella: The glabella, the area between the eyebrows, is the second most dangerous zone. The supratrochlear and supraorbital arteries traverse this region and directly connect to the ophthalmic circulation, increasing the risk of retrograde embolisation [10]. Treatments targeting frown lines in this area require extreme precision.
- Forehead: The forehead, including the temporal region, represents another high-risk zone. The supraorbital and supratrochlear arteries and their branches course through this area, directly communicating with the ophthalmic circulation [11]. Forehead filler treatments for wrinkle reduction and contouring demand heightened caution.
- Periorbital Region: The periorbital region, surrounding the eyes, is also considered a high-risk area. The angular artery, supratrochlear artery, and zygomaticofacial arteries in this region are close to the ophthalmic artery and its branches [12]. Procedures targeting brow lifts and upper eyelid rejuvenation require careful consideration of vascular anatomy.
- Cheeks and Lower Eyelids: While less commonly reported, the cheeks and lower periorbital areas also carry a risk. The infraorbital branches of the maxillary artery and the angular artery in the midface region are interconnected with the ophthalmic artery network [13]. Tear trough filler treatments that address under-eye hollows require meticulous technique.
These high-risk zones are characterised by a dense concentration of arteries and anastomoses, which increase the likelihood of inadvertent intravascular injection and create pathways for emboli to reach the ophthalmic artery. Practitioners must possess a detailed three-dimensional understanding of facial vascular anatomy, visualising the course of arteries and veins and appreciating individual anatomical variations. Thorough anatomical knowledge, combined with meticulous injection technique, is the cornerstone of minimising the risk of blindness after dermal fillers.
Preventative Measures: A Multifaceted Approach to Minimising Risk
While the statistical probability of blindness after dermal fillers remains low, the catastrophic nature of this complication necessitates a proactive and multifaceted approach to risk minimisation. Practitioners are primarily responsible for safeguarding patient safety through rigorous training, adherence to best practices, and a commitment to continuous learning. Key preventative measures include:
- Comprehensive Anatomical Knowledge: A thorough understanding of facial vascular anatomy is a non-negotiable prerequisite for any practitioner performing dermal filler injections. This extends beyond basic textbook knowledge to encompass a detailed three-dimensional understanding of the course, depth, and branching patterns of facial arteries and veins. Practitioners must be able to visualise the intricate vascular network beneath the skin, appreciate individual anatomical variations, and identify high-risk zones with precision. Resources such as anatomical atlases, cadaveric dissections, and advanced imaging techniques like ultrasound can enhance anatomical knowledge and spatial awareness.
- Aspiration Technique: Aspiration, the act of pulling back on the syringe plunger before injecting, is a critical step in attempting to detect intravascular placement. While not foolproof, aspiration aims to confirm that the needle tip is not within a blood vessel before filler is injected. A positive aspiration, indicated by blood entering the syringe, should immediately halt the injection. However, it is crucial to acknowledge the limitations of aspiration. False negatives can occur due to small needle gauges, high-viscosity fillers, vessel collapse, or the needle bevel partially within a vessel. A negative aspiration does not guarantee extravascular placement, but a positive aspiration is a clear warning sign that must be heeded.
- Slow, Low-Pressure Injection: Injecting filler slowly and with minimal pressure significantly reduces the likelihood of retrograde flow and vascular embolisation. Rapid injection and high pressure can force filler material into blood vessels, increasing the risk of occlusion. Slow, controlled injection allows for real-time observation of tissue response and minimizes the risk of vascular compromise. Practitioners should continuously monitor the injection site for blanching, pain, or other signs of vascular occlusion during the procedure.
- Appropriate Needle/Cannula Selection: The choice between needles and cannulas, as well as the appropriate gauge, can influence the risk of intravascular injection. With their blunt tips, Cannulas are generally considered to offer a degree of reduced risk compared to sharp needles, particularly for larger vessels in deeper tissue planes. Cannulas are thought to be less likely to puncture blood vessels due to their blunt nature, gliding past vessels rather than piercing them. However, cannulas are not without risk, and intravascular injection can still occur, especially with smaller gauge cannulas or in areas with dense vascular networks. Needles, while carrying a higher risk of vascular puncture, offer greater precision and control, particularly for superficial injections and delicate areas. The choice between needles and cannulas should be based on the practitioner’s experience, the specific anatomical area being treated, the filler properties, and the desired injection depth.
- Product Knowledge and Rheology: Understanding the properties of the filler being used, including its viscosity, elasticity, and cohesivity, is crucial for controlled and precise placement. Highly viscous fillers, while offering structural support and longevity, may also pose a greater risk of vascular occlusion if inadvertently injected intravascularly due to their cohesive nature and potential to form larger emboli. Practitioners should be familiar with the rheological properties of the fillers and select products appropriate for the intended treatment area and injection technique.
- Avoid High-Risk Areas Where Possible: In certain cases, particularly for novice practitioners or when addressing non-essential aesthetic concerns, avoiding high-risk areas altogether may be the safest strategy. If treatment in high-risk zones is deemed necessary, practitioners should exercise extreme caution, employ meticulous technique, and ensure they are adequately trained and experienced to manage potential complications. Alternative treatment areas or modalities with a lower risk profile should be considered whenever appropriate.
While no single preventative measure can completely eliminate the risk of blindness after dermal fillers, a comprehensive approach combining these strategies significantly reduces the likelihood of this devastating complication. Continuous education, rigorous training, and unwavering adherence to best practices are paramount for ensuring patient safety in aesthetic medicine.
Recognising and Responding to Vascular Occlusion: Activating the Emergency Protocol
Prompt recognition and immediate response are crucial in cases of suspected vascular occlusion following dermal filler injection. Time is of the essence, as retinal ischaemia can lead to irreversible vision loss within minutes. Practitioners must be vigilant in identifying warning signs during and immediately after the procedure and have a clear and well-rehearsed emergency protocol in place. Key warning signs include:
- Sudden, Severe Pain: Disproportionate and escalating pain during injection, often described as intense and unlike typical injection discomfort, is a significant red flag.
- Skin Blanching: Abrupt pallor or whitening of the skin in the injection area, indicating vascular compromise and reduced blood flow.
- Visual Disturbances: Any sudden onset of visual disturbances, including blurred vision, diplopia (double vision), visual field defects, or sudden vision loss in one eye, must be treated as a medical emergency.
- Eye Pain: Ocular pain, often described as intense and radiating, can indicate ophthalmic artery involvement.
- Nearby Skin Ischaemia: Blanching or livedo reticularis (a net-like purplish discoloration) in the skin surrounding the injection site can indicate vascular compromise extending beyond the immediate injection area.
- Ophthalmoplegia: Weakness or paralysis of the extraocular muscles, leading to impaired eye movement, double vision, or strabismus (misalignment of the eyes).
- Ptosis: Drooping eyelid, indicating potential nerve or muscle compromise.
- Neurological Symptoms: In some cases, vascular occlusion can extend to cerebral circulation, leading to stroke-like symptoms such as unilateral weakness, numbness, speech difficulties, dizziness, nausea, or an altered level of consciousness.
Upon recognising any of these warning signs, practitioners must immediately activate their emergency protocol:
- Stop Injecting Immediately: Halt the injection procedure immediately to prevent further filler administration and potential embolisation.
- Assess the Patient: Conduct a rapid assessment of the patient’s symptoms, including visual acuity, pupillary reflexes, and extraocular movements. Document the specific symptoms and their onset.
- Call for Emergency Assistance: Contact an ophthalmologist or emergency eye care specialist immediately for urgent consultation and potential referral. Time is critical, and prompt ophthalmological intervention is paramount.
- Initiate Emergency Measures: While awaiting specialist consultation, initiate immediate office-based interventions to potentially restore blood flow. These may include:
- Ocular Massage: Gentle, rhythmic ocular massage may help dislodge emboli and improve retinal perfusion.
- Breathing into a Paper Bag: To increase carbon dioxide levels in the blood, inducing vasodilation and potentially improving blood flow to the retina.
- Topical Nitroglycerin: Applying topical nitroglycerin paste to the affected area may promote vasodilation and improve blood flow.
- Aspirin: Administering 300mg of aspirin may help prevent further clot formation and improve blood flow.
- Ocular Hypotensive Agents: Topical timolol eye drops or oral acetazolamide may be considered to lower intraocular pressure and improve retinal perfusion.
- Prepare for Hyaluronidase Administration (for HA Fillers): In cases involving HA fillers, prepare for immediate hyaluronidase injection, which is the most logical intervention. Have hyaluronidase readily available and be prepared to administer high doses.
- Provide Psychological Support: Reassure the patient and communicate clearly and honestly about the situation and the steps being taken. Acknowledge the seriousness of the situation while maintaining a calm and reassuring demeanour.
- Document Everything: Meticulously document all findings, interventions, and communications with specialists and the patient. This documentation is crucial for medical records and potential medico-legal considerations.
It is crucial to emphasise that these measures are temporising steps while awaiting specialist ophthalmological intervention. They should not delay or replace immediate referral to an emergency eye care facility. In cases of suspected blindness after dermal fillers, time is vision, and a swift, coordinated response is essential to maximise the chances of a positive outcome.
Treatment Strategies: Navigating the Complexities of Filler-Induced Blindness
The management of established blindness after dermal fillers presents significant therapeutic challenges. Despite various treatment modalities explored, no universally effective protocol exists, and outcomes often remain poor. Treatment strategies, as highlighted in the clinical papers, are multifaceted and frequently involve a combination of approaches:
- Immediate Interventions: These initial measures, initiated immediately upon suspicion of vascular occlusion, aim to rapidly restore blood flow rapidly and mitigate ischaemic damage. Ocular massage, breathing into a paper bag, and topical nitroglycerin are considered first-line interventions, although their efficacy in reversing blindness remains unproven in robust clinical trials.
- Hyaluronidase Injection: High-dose hyaluronidase injections represent the most logical and evidence-based intervention for HA fillers. Prompt administration of hyaluronidase, ideally within the first few hours of occlusion, is crucial to maximise its potential to dissolve the HA embolus and restore blood flow. The optimal route of administration remains debated. While subcutaneous injections at the filler site are standard practice, some practitioners advocate for more targeted approaches like supraorbital or retrobulbar injections in severe cases of blindness, aiming to deliver hyaluronidase closer to the ophthalmic artery. Retrobulbar hyaluronidase injection, a technically challenging procedure involving injection behind the eyeball, carries its own risks and remains controversial due to limited evidence of efficacy and potential complications. Supraorbital hyaluronidase injection, targeting the supraorbital artery, is considered less invasive and potentially effective in cases where the blockage is closer to the surface. However, both retrobulbar and supraorbital injections require specialist expertise and carry inherent risks.
- Medical Treatments: Various medical treatments have been explored to support retinal perfusion and mitigate ischaemic damage. These include:
- Corticosteroids: To reduce inflammation and potentially improve blood flow.
- Antiplatelet Therapy: Aspirin and other antiplatelet agents to prevent clot propagation and improve blood flow.
- Carbonic Anhydrase Inhibitors: Acetazolamide to lower intraocular pressure and potentially enhance retinal perfusion.
- Beta-Blockers: Timolol eye drops to lower intraocular pressure.
- Advanced Interventions: In more severe or refractory cases, advanced interventions have been explored, including:
- Hyperbaric Oxygen Therapy (HBOT): HBOT aims to increase oxygen delivery to ischaemic tissues and potentially improve retinal survival. While some case reports suggest potential benefit, robust evidence supporting its efficacy in reversing blindness after dermal fillers is lacking.
- Anterior Chamber Paracentesis: A procedure to lower intraocular pressure by draining aqueous humour from the anterior chamber of the eye, aiming to improve retinal perfusion.
- Energy-Based Treatments: Energy-based treatments, such as laser therapy, have been explored with limited and inconsistent results.
- Intra-arterial Thrombolysis and Hyaluronidase: Selective intra-arterial hyaluronidase, administered via interventional radiology and combined with intra-arterial fibrinolytic agents, has shown some promise in achieving partial visual recovery in a limited number of cases. However, this approach is highly complex and invasive and carries significant risks, including stroke and haemorrhage. Its use remains limited to specialised centres with interventional radiology capabilities.
Clinical papers consistently highlight the limited success of current treatment strategies for filler-induced blindness. Outcomes remain poor in the majority of cases, with permanent vision loss being a frequent consequence, even with aggressive intervention. This underscores the importance of prevention as the most effective strategy to protect patients from this devastating complication.
Patient Education and Informed Consent – Empowering Patients Through Knowledge
Blindness after dermal fillers is a stark and sobering reminder that even seemingly minor cosmetic procedures carry inherent risks. Ethical and legal imperatives demand that patients are fully informed of these risks, including the most serious complication of blindness, before undergoing treatment. Comprehensive informed consent is not merely a formality; it is a cornerstone of patient safety and empowers patients to make autonomous and informed decisions about their care.
Informed consent discussions must explicitly mention the risk of vision loss, clearly stating that blindness after dermal fillers, while rare, is a potential complication. The consent process should be thorough, transparent, and tailored to the individual patient, ensuring they understand the nature of the procedure, the potential benefits, and the possible risks, including:
- Specific Risks Based on Injection Area: Clearly explain the increased risk associated with high-risk zones like the nose, glabella, and forehead. Utilise visual aids, such as anatomical diagrams, to illustrate the vascular pathways and risk areas in an accessible way.
- Severity and Irreversibility of Blindness: Emphasise the potentially devastating and irreversible nature of filler-induced blindness. Patients should understand that treatments for blindness after dermal fillers have limited effectiveness, and vision loss may be permanent.
- Limitations of Treatment: Discuss the limitations of current treatment options for filler-induced blindness and the often poor visual outcomes despite intervention.
- Importance of Choosing Qualified Practitioners: Stress the importance of choosing qualified, experienced, and appropriately trained practitioners who prioritise patient safety above all else. Explain the significance of anatomical knowledge, meticulous technique, and adherence to best practices in minimising risk.
- Alternatives to Dermal Fillers: If appropriate, discuss alternative treatment options, particularly for high-risk areas, allowing patients to consider less risky approaches to aesthetic enhancement.
Practitioners must resist any pressure to minimise discussion of serious complications, even if they believe it might alarm patients. Valid informed consent necessitates full disclosure of material risks, allowing patients to make genuinely informed decisions about their treatment and empowering them to weigh the potential benefits against the potential, albeit rare, risks.
Conclusion
While blindness after dermal fillers is a rare event, it represents one of the most devastating complications in aesthetic medicine. Its permanent and life-altering nature demands serious attention from all practitioners performing filler injections. The pursuit of aesthetic enhancement must never overshadow patient safety and a complete understanding of potential risks, however infrequent they may be.
This article has explored the anatomical mechanisms underlying filler-induced blindness, highlighted high-risk areas, outlined preventative strategies, reviewed management protocols, and emphasised the critical importance of patient education and informed consent. Key take-away messages for practitioners include:
- Prioritise Prevention: To minimise the risk of intravascular injection, focus on meticulous injection technique, comprehensive anatomical knowledge, and adherence to best practices.
- Be Vigilant: Recognise early warning signs of vascular occlusion and have a well-rehearsed emergency protocol in place.
- Act Swiftly: In cases of suspected blindness, act swiftly and decisively, initiating immediate office-based interventions and seeking urgent ophthalmological consultation.
- Empower Patients: Provide comprehensive informed consent, ensuring patients are fully aware of the potential risks, including blindness, and are empowered to make informed decisions.
- Stay Informed: Continuously update knowledge on best practices, emerging techniques, and evolving treatment protocols for managing filler complications.
Open communication, rigorous training, unwavering adherence to best practice, and a commitment to continuous learning are the cornerstones of minimising the risk of blindness after dermal fillers and ensuring patient well-being within the realm of aesthetic medicine. As research continues to evolve, practitioners must stay abreast of the latest evidence to minimise the occurrence of this devastating complication and ensure that patient safety remains paramount.
References
Rzany B, DeLorenzi C. The Science of Hyaluronidase and Its Application in Aesthetic Practice. J Clin Aesthet Dermatol. 2023 Jul;16(7 Suppl 1):S1-S2.
Goodman GJ, Magnusson MR, Callan P, et al. A consensus on minimizing the risk of hyaluronic acid embolic visual loss and suggestions for immediate bedside management. Aesthetic Surg J. 2020 Sep 14;40(9):1009-1021.
Walker L, Convery C, Davies E, et al. Consensus opinion for the management of soft tissue filler-induced vision loss. J Clin Aesthet Dermatol. 2021 Jun;14(6):E84-E94.
Soares DJ, Bowhay A, Blevins LW, et al. Patterns of filler-induced facial skin ischemia: a systematic review of 243 cases and introduction of the FOEM scoring system and grading scale. Plast Reconstr Surg. 2023 Mar 1;151(3):592e-608e.
Bravo BSF, Cavalcante T, Silveira C, et al. Resolve and dissolve—An ultrasound-guided investigation on the effects of hyaluronidase on different soft tissue fillers. J Cosmet Dermatol. 2024;23(5):3173-3181.
Kroumpouzos G, Treacy P. Hyaluronidase for Dermal Filler Complications: Review of Applications and Dosage Recommendations. JMIR Dermatol 2024;7:e50403.
Soares DJ, Bravo BSF. Cosmetic Filler–Induced Vascular Occlusion: A Rising Threat Presenting to Emergency Departments. Ann Emerg Med. 2024 Jan;83(1):59-67.
Hong G-W, Hu H, Chang K, et al. How Should We Use Hyaluronidase for Dissolving Hyaluronic Acid Fillers?. J Cosmet Dermatol. 2025;24:e16783.
Friedman R, Coombs AV, Stevens S, et al. Complete Vision Recovery After Filler-Induced Blindness Using Hyperbaric Oxygen Therapy: Case Report and Literature Review. Aesthet Surg J Open Forum. 2024 Apr 27;2024:ojae036.