Introduction
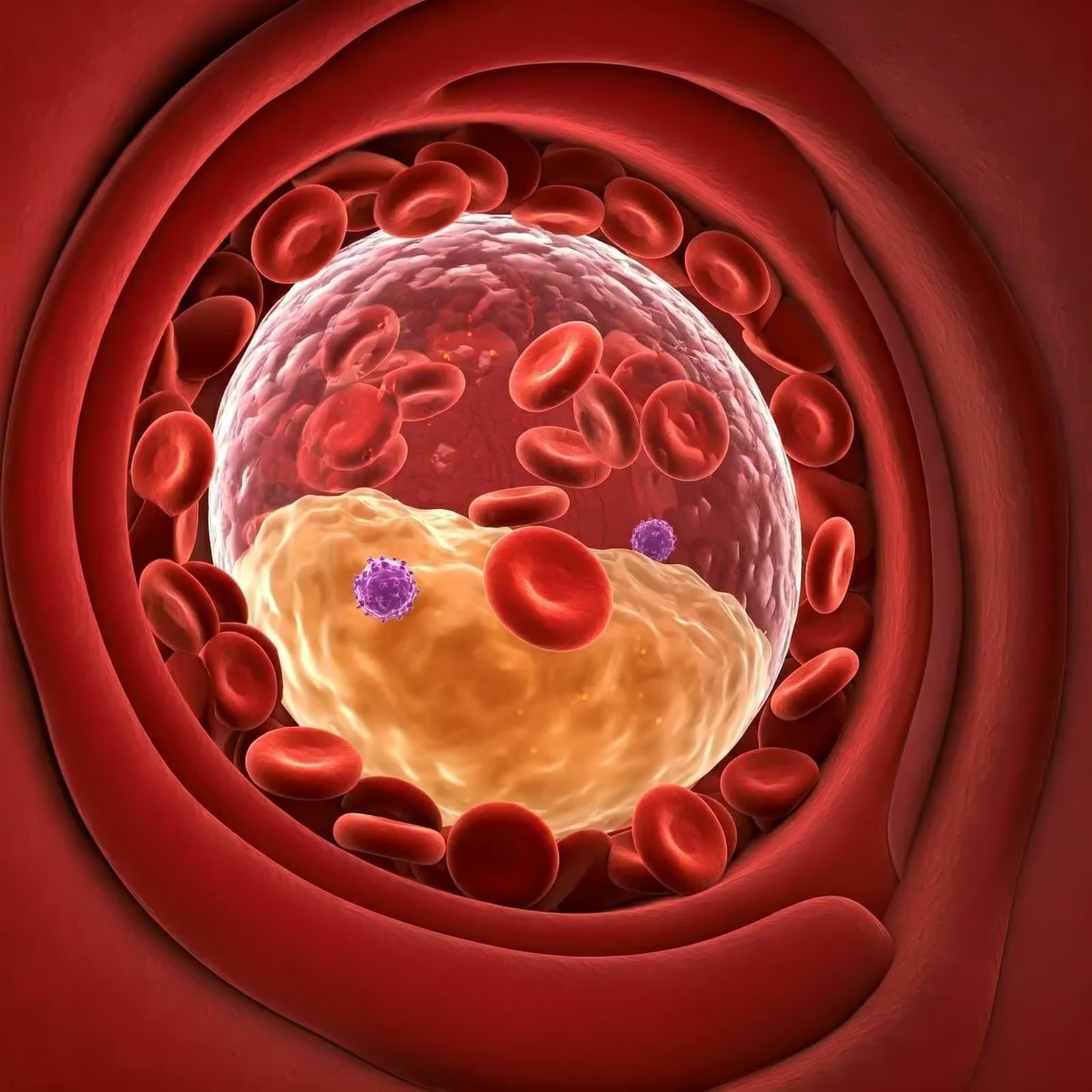
Dermal filler injections have become a cornerstone of aesthetic medicine, providing a minimally invasive solution for rejuvenating facial features, addressing volume loss, and smoothing wrinkles. Despite their widespread popularity and general safety profile, complications can arise, with vascular occlusion being one of the most serious. This condition occurs when filler material inadvertently enters an artery, obstructing blood flow and leading to potentially devastating outcomes, including skin necrosis, scarring, and even blindness.
The glabella, the area between the eyebrows, poses an exceptionally high risk for vascular occlusion due to its complex vascular anatomy and the proximity of critical arteries that supply the eyes and surrounding structures. This comprehensive review delves into the mechanisms, diagnosis, management, and prevention of forehead vascular occlusion caused by dermal fillers in the glabella region. A thorough understanding of this complication is essential for practitioners to effectively enhance patient safety and mitigate risks.
Relevant Anatomy in Forehead Vascular Occlusion
A detailed understanding of the glabella’s vascular anatomy is crucial for safe injection practices. The primary blood supply to this region arises from the supratrochlear and supraorbital arteries, both branches of the ophthalmic artery. These arteries emerge from the orbit and ascend along the forehead, supplying the skin, muscles, and subcutaneous tissues.
- Supratrochlear Artery: Exiting the orbit at the superior medial angle of the eyebrow, it courses vertically upward, supplying the medial forehead.
- Supraorbital Artery: Emerging from the supraorbital notch or foramen located at the superior orbital rim, this artery runs superolaterally on the forehead, supplying the lateral forehead and scalp.
Both arteries originate from the ophthalmic artery, which arises from the internal carotid artery—a major vessel responsible for supplying the brain and eyes. The glabella’s intricate vascular network, combined with limited collateral circulation, amplifies the risk of complications if blood flow is disrupted. Vascular occlusion in this region can lead to tissue necrosis, scarring, and, in severe cases, ocular complications.
Mechanisms of Forehead Vascular Occlusion
Vascular occlusion during dermal filler injection results from filler material inadvertently entering an artery, obstructing blood flow. This can occur through several mechanisms:
- Direct Intra-Arterial Injection: The filler is directly deposited into the arterial lumen, blocking blood flow.
- Retrograde Flow: The filler travels backwards into larger arterial branches, causing an upstream obstruction.
- External Compression: The filler material exerts pressure on the vessel externally, restricting blood flow.
Several factors increase the risk of vascular occlusion:
- Injection Pressure: High injection pressure can force filler into an artery.
- Filler Properties: Viscosity and cohesivity of the filler influence its potential to block vessels.
- Anatomical Variations: Individual differences in arterial anatomy may heighten the risk.
- Technique: Poor injection practices, such as deep injections.
Clinical Presentation
The signs and symptoms of vascular occlusion can vary depending on the affected artery, its severity, and the extent of collateral circulation. Prompt recognition of these symptoms is critical for timely intervention.
Immediate Signs
- Pain: Intense, often radiating along the affected artery.
- Blanching: Skin appears pale or white due to interrupted blood flow.
- Delayed Capillary Refill: Prolonged time for colour to return when the skin is pressed.
- Paraesthesia: Tingling or numbness in the affected area due to nerve compression.
Delayed Signs
- Skin Discolouration: Progression from blanching to cyanosis (bluish hue).
- Blistering and Necrosis: Severe cases may result in skin death, forming black eschars.
- Visual Disturbances: Blurred vision or blindness if the ophthalmic artery is involved.
Consequences of Forehead Vascular Occlusion
The consequences of forehead vascular occlusion range from mild and reversible to severe and permanent.
Skin Effects
- Necrosis: Tissue death requiring surgical intervention in severe cases.
- Scarring: Even with successful treatment, scarring may occur.
- Pigmentation Changes: Hypopigmentation or hyperpigmentation in the affected area.
Ocular Complications
- Visual Impairment: From transient vision loss to permanent blindness.
- Anterior Ischaemic Optic Neuropathy (AION): Insufficient blood supply to the optic nerve head.
- Retinal Emboli: Filler particles lodging in retinal vessels, obstructing blood flow.
Diagnosis
Clinical Features
A thorough history and physical examination are essential. Key diagnostic features include:
- Recent filler injection in the glabella.
- Symptoms such as blanching, pain, and delayed capillary refill.
Imaging
- Doppler Ultrasound: Identifies areas of occlusion and assesses blood flow, aiding diagnosis.
Management of Vascular Occlusion
Immediate Treatment
- Stop Injection: Cease injecting immediately.
- Massage: Gentle massage to disperse filler.
- Warm Compresses: Promote vasodilation.
- Hyaluronidase: Inject into the affected area to dissolve hyaluronic acid fillers.
- Pharmacological Interventions: Aspirin and nitroglycerin paste to improve blood flow.
- Hyperbaric Oxygen Therapy: Considered in severe cases to enhance oxygen delivery to tissues.
Delayed Treatment
- Surgical Intervention: Debridement and skin grafting for necrotic areas.
- Ophthalmological Care: Immediate attention for visual symptoms.
Aftercare
Immediate Post-Treatment
- Apply warm compresses regularly.
- Avoid makeup and strenuous activity.
- Use pain relievers as needed.
Long-Term Care
- Protect the area with sunscreen.
- Employ gentle skincare routines post-healing.
Prevention of Vascular Occlusion
Key Strategies
- Thorough Anatomical Knowledge: Master the glabella’s vascular anatomy.
- Injection Technique: Use small boluses, aspirate, and inject slowly..
- Patient Education: Inform patients of risks, signs, and symptoms of occlusion.
Valid Consent
A robust informed consent process includes:
- Explanation of Material Risks: Highlighting vascular occlusion and potential blindness.
- Alternatives: Discussing non-invasive options.
- Documentation: Recording the consent process thoroughly.
Utilising Ultrasound for Prevention
Ultrasound guidance enhances safety by allowing visualisation of arterial structures, improving injection accuracy, and reducing the risk of vascular compromise.
Conclusion
Vascular occlusion in the glabella is a rare but significant complication of dermal filler injections. Early recognition, precise management, and meticulous injection techniques are vital for preventing serious outcomes. By leveraging ultrasound technology and prioritising informed consent, practitioners can ensure safer outcomes and uphold the highest standards in aesthetic medicine.
Frequently Asked Questions (FAQs)
1. What is vascular occlusion, and how does it occur during dermal filler injections?
Vascular occlusion occurs when filler material enters a blood vessel, obstructing blood flow. This can happen through direct intra-arterial injection, retrograde flow, or external compression of the vessel. The blockage prevents oxygen and nutrients from reaching the surrounding tissues, potentially causing severe complications such as tissue necrosis or blindness.
2. Why is the glabella area considered high-risk for forehead vascular occlusion?
The glabella region is high-risk due to its intricate vascular anatomy, primarily supplied by the supratrochlear and supraorbital arteries, which are branches of the ophthalmic artery. These vessels are closely linked to the blood supply of the eyes, making vascular compromise in this area particularly dangerous. Limited collateral circulation further increases the risk of tissue damage and ocular complications.
3. What are the immediate symptoms of vascular occlusion?
Early signs include:
- Intense pain at the injection site or along the artery.
- Blanching or whitening of the skin.
- Delayed capillary refill when the skin is pressed.
- Numbness or tingling in the affected area.
Recognising these symptoms promptly is crucial to preventing severe complications.
4. How can practitioners prevent vascular occlusion during filler injections?
Prevention strategies include:
- Thorough anatomical knowledge of vascular structures.
- Using cannulas to minimise vessel penetration.
- Injecting slowly and aspirating before each injection to ensure the needle is not in a vessel.
- Using ultrasound guidance for visualisation of blood vessels.
- Avoiding high-pressure injections and large filler volumes.
5. What role does ultrasound guidance play in dermal filler safety?
Ultrasound allows real-time visualisation of vascular structures, ensuring precise needle placement and reducing the risk of intra-arterial injections. It can also assess blood flow in arteries, guide filler placement, and provide immediate feedback, significantly enhancing procedural safety.
6. Can vascular occlusion from dermal fillers cause blindness?
Yes, vascular occlusion involving the ophthalmic artery or its branches can lead to blindness. If filler material blocks the central retinal artery, it cuts off blood supply to the retina, resulting in irreversible damage. Blindness can occur within minutes, making this a medical emergency that requires immediate intervention.
7. How is vascular occlusion treated once it occurs?
Management includes:
- Stopping the injection immediately.
- Massaging the area gently to disperse the filler.
- Applying warm compresses to promote vasodilation.
- Administering hyaluronidase to dissolve hyaluronic acid fillers.
- Using adjunct treatments like aspirin, nitroglycerin paste, or hyperbaric oxygen therapy.
Delayed cases may require surgical debridement or skin grafting for necrotic tissue, while ocular involvement demands urgent ophthalmological evaluation.
8. How long does it take for forehead vascular occlusion to cause tissue necrosis?
Tissue necrosis can develop within hours if blood flow is not restored promptly. Early symptoms, such as blanching and pain, can appear immediately, but the progression to cyanosis and necrosis may take 6–12 hours. Prompt intervention is critical to minimising tissue damage.
9. Are there long-term effects of vascular occlusion if treated promptly?
With timely and effective treatment, full recovery is often possible. However, severe cases may leave long-term effects, such as:
- Scarring or disfigurement.
- Pigmentation changes in the skin (hyperpigmentation or hypopigmentation).
- Permanent visual impairment if the ophthalmic artery is involved.
10. Is it safe to use dermal fillers in the glabella area?
Dermal fillers can be safely used in the glabella by experienced practitioners with thorough anatomical knowledge and a strong emphasis on safety protocols. Using ultrasound guidance, adopting careful injection techniques, and obtaining informed consent is essential for minimising risks. While the glabella is a high-risk area, following best practices can significantly reduce the likelihood of complications.
References
- Beleznay, K., Carruthers, J. D., Humphrey, S., Jones, D., Klein, A. W., & Narurkar, V. A. (2015). Avoiding and treating blindness from fillers: A review of the world literature. Dermatologic Surgery, 41(10), 1097.
- Beleznay, K., Carruthers, J. D., Humphrey, S., & Jones, D. (2014). Update on avoiding and treating blindness from fillers: Injection anatomy and prevention. Dermatologic Surgery, 40(12), 1212–1219.
- Alam, M., Gladstone, H. B., Kramer, E. M., et al. (2014). Techniques for the prevention and treatment of dermal filler complications. Dermatologic Surgery, 40(12), 1251–1258.
- DeLorenzi, C. (2014). Complications of injectable fillers, part 2: Vascular complications. Aesthetic Surgery Journal, 34(4), 584–600.
- Beleznay, K., Carruthers, J. D., Humphrey, S., Jones, D., & Wong, J. K. (2015). Blindness caused by cosmetic filler injection: A review of cause and therapy. Plastic and Reconstructive Surgery, 135(6), 1416–1426.
- Carruthers, J. D., & Carruthers, A. (2005). Injectable soft-tissue fillers: Overview of clinical use. Dermatologic Surgery, 31(Suppl 1), 1606–1613.
- Pavicic, T., & Webb, K. L. (2013). Using facial anatomy to improve dermal filler safety. Aesthetic Medicine, 2(2), 51–56.
- Coleman, S. R., & Saboeiro, A. P. (2001). Fat grafting to the face: Aesthetic surgery with long-term results. Clinics in Plastic Surgery, 28(1), 111–119.
- Dayan, S. H., Arkins, J. P., & Brindise, R. T. (2017). Soft tissue fillers and bio-stimulatory injectables: An integrated approach. Facial Plastic Surgery Clinics of North America, 25(1), 57–67.
- Rzany, B., & Zielke, H. (2010). Complications in dermal filler applications. Journal of Cutaneous and Aesthetic Surgery, 3(1), 10–13.
- Sundaram, H., & Voigts, B. (2017). An evidence-based review of the pharmacology of fillers for facial soft tissue augmentation. Dermatologic Surgery, 43(1), 41–54.
- Hirsch, R. J., Stier, M. A., & Cohen, J. L. (2007). Soft tissue augmentation with fillers. Journal of Drugs in Dermatology, 6(10), 1029–1038.
- Urdiales-Gálvez, F., De Cabo-Francés, F. M., Fernandez-Sanchez, M., & Delgado, N. E. (2017). Managing complications associated with injectable soft-tissue fillers. Plastic and Reconstructive Surgery, 139(4), 787e–795e.
- Jones, D., & Murphy, D. K. (2013). Voluma: A new option for long-lasting volume correction in the midface. Aesthetic Surgery Journal, 33(6 Suppl), S23–S30.
- Signorini, M., Liew, S., Sundaram, H., et al. (2016). Global aesthetics consensus: Avoidance and management of complications from hyaluronic acid fillers—Evidence- and opinion-based review and consensus recommendations. Plastic and Reconstructive Surgery, 137(6), 961e–971e.