Mastering Lip Augmentation: Safe Lip Filler Injection Technique to Prevent Vascular Occlusion
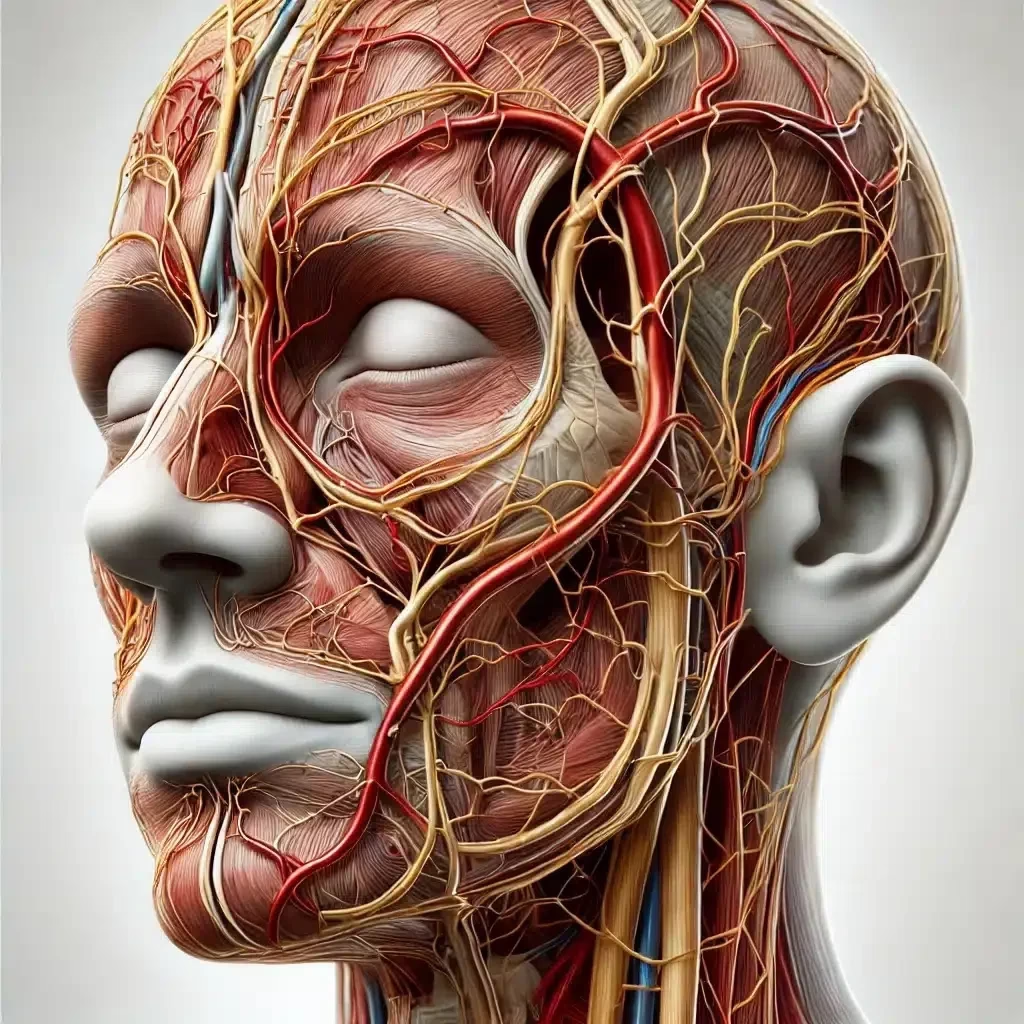
Abstract: Understanding the intricate anatomy of the lips is crucial for clinicians performing dermal filler injections. The superior and inferior labial arteries are vital structures supplying blood to the lips and surrounding tissues. Comprehensive knowledge of their precise locations in relation to the wet/dry border, the vermilion, and the body of the lip is essential to minimise risks such as vascular occlusion during aesthetic procedures. This article synthesises current anatomical insights, incorporating findings from recent clinical studies, to focus specifically on safe injection points that avoid vascular complications. Furthermore, it elaborates on best practices for managing complications, emphasising early recognition and appropriate intervention.

Introduction
Lip augmentation has become increasingly popular in aesthetic medicine, necessitating a profound understanding of lip anatomy to ensure patient safety and optimal outcomes. Vascular complications, although rare, can lead to serious consequences such as tissue necrosis or even blindness. The superior and inferior labial arteries play a pivotal role in these risks due to their variable anatomy and proximity to common injection sites.
Anatomy of the Labial Arteries
Superior Labial Artery
The superior labial artery originates from the facial artery, which branches from the external carotid artery. It traverses medially along the upper lip, supplying blood to the upper lip tissues, including the vermilion and the orbicularis oris muscle.
- Course and Location: Cotofana et al. (2020) utilised ultrasound imaging to map the three-dimensional pathway of the superior labial artery. The artery predominantly runs within the submucosal plane (58.5% of cases) at an average depth of 5.6 ± 0.13 mm from the skin surface. In the midline, it courses within the red lip (vermilion zone) in all investigated individuals, highlighting a critical risk area for injections[^1^].
- Variations in Depth and Pathway: Lee et al. (2020) found that the superior labial artery could be located as superficially as 3.2 mm from the mucosal surface, with its position varying between individuals[^2^]. This variability necessitates careful consideration of injection depth.
- Three-Dimensional Anatomy in Chinese Individuals: Zhu et al. (2024) conducted a computed tomography (CT) scanning study in Chinese individuals, revealing that the superior labial artery often follows a tortuous path with multiple branches, increasing the complexity of safe injection practices in this population[^3^].
Inferior Labial Artery
The inferior labial artery also branches from the facial artery and supplies blood to the lower lip.
- Course and Location: According to Cotofana et al. (2020), the inferior labial artery typically traverses medially within the lower lip, primarily within the submucosal plane (58.5%), at an average depth of 5.2 ± 0.14 mm from the skin surface[^1^].
- Anatomical Variations: Lee et al. (2020) reported that the inferior labial artery might be located as close as 2.9 mm from the mucosal surface, emphasising the need for cautious injection techniques in the lower lip[^2^].
- Typical Patterns: Tansatit et al. (2014) observed that the inferior labial artery commonly presents a consistent pattern, running along the wet-dry border, which is crucial information for practitioners aiming to avoid vascular injury[^4^].
Anatomical Variations and Their Significance
Variability in Labial Arteries
Anatomical variations in the labial arteries significantly impact the safety of lip augmentation procedures.
- Literature Review Findings: Samizadeh et al. (2019) compiled data on the variability of labial artery anatomy, noting that the arteries may present as single or multiple branches, with differences in depth and relation to muscular and mucosal structures[^5^]. Such variability necessitates an individualised approach to each patient.
- Implications for Aesthetic Treatments: Understanding that standard anatomical landmarks may not always correlate with arterial locations is essential. This awareness can guide clinicians to modify injection techniques accordingly.
Three-Dimensional Considerations
- CT Scanning Insights: Zhu et al. (2024) utilised three-dimensional CT scanning to provide a detailed understanding of the superior labial artery’s course in Chinese individuals[^3^]. Their findings suggest that ethnicity may influence arterial patterns, further emphasising the need for personalised treatment plans.
- Comprehensive Anatomical Reviews: Lee et al. (2018) provided a comprehensive review of the facial artery, including its branches to the lips[^6^]. They highlighted that the arteries could have unexpected courses and anastomoses, which could complicate injections if not properly understood.
High-Risk Zones in Dermal Filler Placement
Identifying and understanding high-risk zones is paramount for preventing vascular complications.
- Midline of the Lips
- Arterial Presence: Both the superior and inferior labial arteries course within the red lip at the midline in all individuals studied by Cotofana et al. (2020)[^1^]. This area is highly susceptible to vascular occlusion during injections.
- Vermilion Zone
- Arterial Proximity: With a high frequency of arterial presence within the red lip (upper lip 83%, lower lip 86.2%), injections in the vermilion zone require meticulous technique[^1^].
- Wet-Dry Border
- Arterial Pathway: Tansatit et al. (2014) found that the labial arteries often run along or near the wet-dry border, a common site for filler injections[^4^]. Injecting too deeply in this area increases the risk of arterial injury.
- Ethnic Variations
- Population Differences: Zhu et al. (2024) highlighted differences in arterial anatomy among Chinese individuals, suggesting that practitioners should consider ethnic variations when planning injections[^3^].
Safe Lip Injection Techniques
General Principles
- Superficial Injection Plane
- Clinical Recommendations: Cotofana et al. (2020) advocate for a superficial injection plane for lip volumisation procedures, injecting into the superficial subcutaneous tissue of the cutaneous lip to avoid deeper arteries[^1^].
- Perpendicular Approach
- Technique Advantages: Approaching the lip perpendicularly from the cutaneous side can increase safety, as the arteries are most frequently located within the red lip[^1^].
Upper Lip Techniques
- Avoiding the Vermilion Border
- Technique Modification: Given the superior labial artery’s proximity to the vermilion border, injections should be performed either superficially in the cutaneous lip or deeper in the pre-muscular plane, avoiding the intermediate depth where the artery typically resides.
- Lateral Injection Sites
- Safety Consideration: Tansatit et al. (2014) suggest that the lateral aspects of the upper lip have fewer arterial branches, making them safer for injections[^4^].
Lower Lip Techniques
- Superficial Placement
- Risk Reduction: Injecting superficially into the cutaneous lower lip can reduce the risk of encountering the inferior labial artery[^1^].
- Avoiding Midline Injections
- Technique Adjustment: Since the inferior labial artery is consistently found at the midline within the red lip, injections should be administered laterally or with caution if central enhancement is desired.
Utilising Ultrasonography and Imaging
- Ultrasound Guidance
- Real-Time Visualisation: Lee et al. (2020) emphasise the benefits of ultrasonography in visualising the labial arteries before and during injections[^2^]. This practice allows for real-time adjustments to avoid vascular structures.
- Three-Dimensional Mapping
- Enhanced Safety: Advanced imaging techniques, such as those used by Zhu et al. (2024), enable practitioners to understand individual arterial anatomy better, potentially reducing the risk of complications[^3^].
Anatomical Mapping and Individualised Approaches
- Assessing Anatomical Variations
- Patient Evaluation: Samizadeh et al. (2019) advocate for thorough patient assessments to identify anatomical variations that could impact injection safety[^5^].
- Ethnic and Individual Differences
- Tailored Treatments: Recognising that arterial patterns may vary with ethnicity and individual anatomy is crucial. Practitioners should adjust their techniques accordingly, as suggested by Zhu et al. (2024)[^3^].
Techniques to Enhance Safety
Patient Assessment
- Medical History Review
- Identifying Risks: Reviewing the patient’s medical history for previous lip procedures or vascular anomalies can inform safer injection strategies.
- Physical Examination
- Visual and Palpation Techniques: A careful examination can reveal superficial vessels or structural anomalies.
Product Selection
- Appropriate Fillers
- Viscosity Considerations: Using fillers suitable for superficial placement, with lower viscosity, minimises the risk of vascular compression.
- Hyaluronic Acid Fillers
- Reversibility Advantage: Preferred due to their reversibility with hyaluronidase in case of vascular occlusion.
Injection Techniques
- Micro-Aliquot Technique
- Risk Mitigation: Injecting small amounts incrementally reduces the risk of compressing or occluding a vessel.
- Linear Threading and Retrograde Injection
- Controlled Placement: These techniques allow for precise filler placement and reduce the risk of intravascular injection.
- Use of Blunt-Tip Cannulas
- Safety Enhancement: Cannulas can navigate through tissue planes while displacing vessels, reducing the likelihood of arterial puncture (Scheuer et al., 2022)[^7^].
Managing Complications
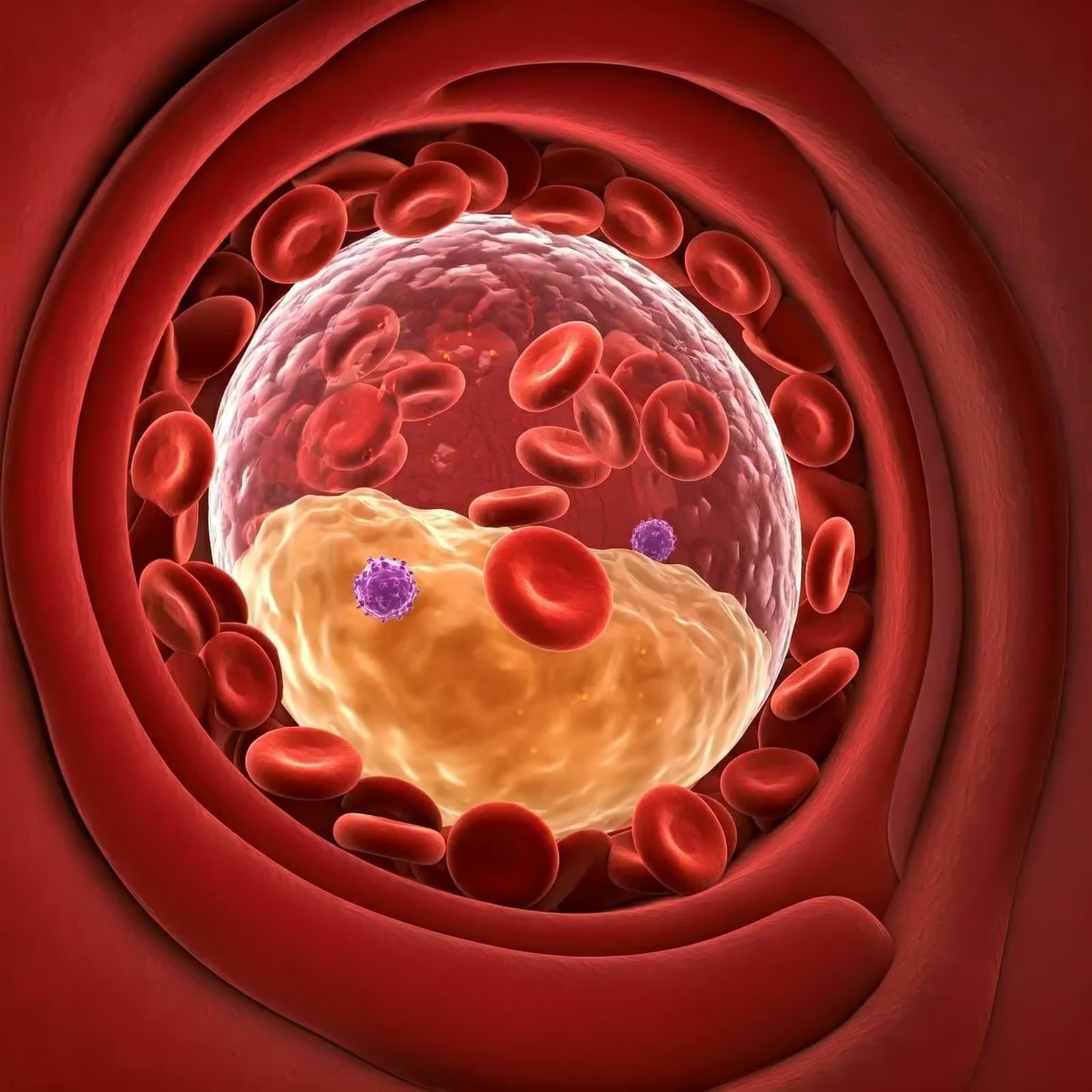
Despite all precautions, complications can occur. Early recognition and prompt management are critical to minimise adverse outcomes.
Early Recognition
- Signs of Vascular Occlusion
- Immediate Indicators:
- Blanching: A sudden whitening of the skin due to compromised blood flow.
- Intense Pain: Disproportionate to the procedure, often described as severe and persistent.
- Colour Changes: Mottling or purplish discolouration indicating impaired circulation.
- Sensory Changes: Numbness or tingling in the affected area.
- Delayed Indicators:
- Skin Coolness: The area may feel cooler due to lack of perfusion.
- Ulceration and Necrosis: Tissue breakdown occurring hours to days after the procedure.
- Importance of Monitoring
- Continuous Observation: The practitioner should monitor the patient during and immediately after the injection for any signs of vascular compromise.
Immediate Intervention
- Cessation of Injection
- First Response: Stop injecting immediately upon suspicion of vascular occlusion to prevent further filler deposition.
- Assessment
- Confirming Diagnosis: Evaluate the affected area for signs of arterial occlusion versus other complications such as allergic reactions or haematoma.
- Massage and Warm Compresses
- Promoting Vasodilation: Gently massaging the area can help disperse the filler. Applying warm compresses increases local blood flow and may aid in relieving vessel compression.
- Hyaluronidase Administration
- Protocol for Use:
- Dosage: Inject 150–300 units of hyaluronidase directly into and around the affected area. The exact dose may vary based on the extent of occlusion and should be adjusted accordingly.
- Technique: Use a small-gauge needle to infiltrate the area thoroughly, ensuring widespread distribution of hyaluronidase.
- Repeat Injections: May be necessary every hour for several hours, depending on the clinical response.
- Mechanism of Action: Hyaluronidase enzymatically degrades hyaluronic acid fillers, reducing the volume of the obstructing material and relieving pressure on the occluded vessel.
- Aspirin Administration
- Antiplatelet Effect: A single dose of 300 mg aspirin may be administered to inhibit platelet aggregation and promote blood flow, unless contraindicated.
- Topical Nitroglycerin
- Vasodilation: Application of nitroglycerin paste can cause local vasodilation, potentially improving perfusion. However, its use should be cautious due to systemic absorption and possible side effects.
Adjunctive Measures
- Oxygen Therapy
- Enhancing Oxygenation: Administering supplemental oxygen can aid tissue oxygenation.
- Systemic Steroids
- Reducing Inflammation: May be considered to decrease inflammatory responses and prevent further tissue damage.
- Low Molecular Weight Heparin
- Preventing Thrombosis: In cases where thrombosis is suspected, anticoagulation therapy may be initiated under specialist guidance.
Specialist Referral and Support
- Consultation with Specialists
- Vascular Surgeon or Dermatologist: Immediate referral to a specialist is advised if there is no improvement or if the occlusion affects critical areas such as the retina.
- Ophthalmology Referral
- Visual Symptoms: If the patient experiences visual disturbances, an urgent ophthalmology assessment is imperative due to the risk of retinal artery occlusion leading to blindness.
Follow-Up Care
- Monitoring Progress
- Regular Assessments: Frequent evaluations to assess the efficacy of interventions and detect any progression of tissue damage.
- Wound Care
- Managing Necrosis: If tissue necrosis occurs, appropriate wound care protocols should be initiated to prevent infection and promote healing.
- Psychological Support
- Patient Counselling: Addressing the emotional impact of complications is essential for patient well-being.
Documentation and Reporting
- Detailed Records
- Clinical Notes: Document all findings, interventions, and patient communications meticulously.
- Incident Reporting
- Regulatory Compliance: Report adverse events to relevant health authorities as required, contributing to collective knowledge and improved practices.
- Informed Consent
- Pre-Procedural Discussions: Ensure that patients are informed about potential risks and complications prior to treatment, with documented consent.
Conclusion
A thorough understanding of the superior and inferior labial arteries’ anatomy is indispensable for safe and effective dermal filler placement in the lips. Clinicians must remain vigilant of high-risk zones and utilise techniques that minimise vascular injury. Incorporating insights from anatomical research, such as those by Cotofana et al. (2020), Zhu et al. (2024), and other key studies, enhances clinical practice and patient safety. By focusing on safe injection points, employing meticulous techniques, and adhering to best practices in managing complications, practitioners can significantly reduce the risk of vascular occlusion, leading to better outcomes and higher patient satisfaction.
References
[^1^]: Cotofana, S., Alfertshofer, M., Schenck, T. L., et al. (2020). Anatomy of the Superior and Inferior Labial Arteries Revised: An Ultrasound Investigation and Implication for Lip Volumization. Aesthetic Surgery Journal, 40(10), 1067–1074. doi:10.1093/asj/sjaa137
[^2^]: Lee, K. L., Lee, H. J., Youn, K. H., & Kim, H. J. (2020). Positional Relationship of Superior and Inferior Labial Artery by Ultrasonography Image Analysis for Safe Lip Augmentation Procedures. Clinical Anatomy, 33(2), 158–164. doi:10.1002/ca.23379
[^3^]: Zhu, G. S., Liao, Z. F., Chen, C. L., et al. (2024). Three-Dimensional Computed Tomography Scanning Study of the Superior Labial Artery in Chinese Individuals for Assessing Filler Injection Safety. Aesthetic Plastic Surgery, 48(19), 3962–3970. doi:10.1007/s00266-024-04187-8
[^4^]: Tansatit, T., Apinuntrum, P., & Phetudom, T. (2014). A Typical Pattern of the Labial Arteries with Implication for Lip Augmentation with Injectable Fillers. Aesthetic Plastic Surgery, 38(6), 1083–1089. doi:10.1007/s00266-014-0401-8
[^5^]: Samizadeh, S., Pirayesh, A., & Bertossi, D. (2019). Anatomical Variations in the Course of Labial Arteries: A Literature Review. Aesthetic Surgery Journal, 39(11), 1225–1235. doi:10.1093/asj/sjy235
[^6^]: Lee, H. J., Won, S. Y., O, J., et al. (2018). The Facial Artery: A Comprehensive Anatomical Review. Clinical Anatomy, 31(1), 99–108. doi:10.1002/ca.23007
[^7^]: Scheuer, J. F., Sieber, D. A., Pezeshk, R. A., et al. (2022). An Illustrated Anatomical Approach to Reducing Vascular Risk During Facial Filler Injections. Plastic and Reconstructive Surgery, 149(2), 321e–332e. doi:10.1097/PRS.0000000000008718
By integrating detailed anatomical knowledge with cautious clinical practice and adhering to best practices in managing complications, clinicians can ensure safer outcomes in dermal filler procedures, enhancing both patient satisfaction and professional confidence.