Introduction
Dermal filler injections have revolutionised the field of aesthetic medicine, offering a minimally invasive approach to facial rejuvenation. Millions worldwide seek these treatments to restore lost volume, smooth wrinkles, and enhance facial contours. However, like any medical procedure, dermal filler injections are not without potential side effects. Post-treatment dermal filler swelling is one of the most common and concerning side effects.
This article aims to provide a comprehensive overview of dermal filler swelling following dermal filler treatments. We will explore its causes and the role of ultrasound in diagnosis and management, and provide evidence-based strategies for mitigation. Additionally, we will delve into specific considerations for tear trough filler and the crucial role of hyaluronidase in managing complications.

Understanding Post-Filler Swelling: A Multifaceted Issue
Swelling after dermal filler injection is a complex phenomenon driven by a confluence of factors. While often considered a normal and self-limiting response, understanding the underlying mechanisms is crucial for both practitioners and patients.
The Mechanics of Injection Trauma and the Inflammatory Cascade
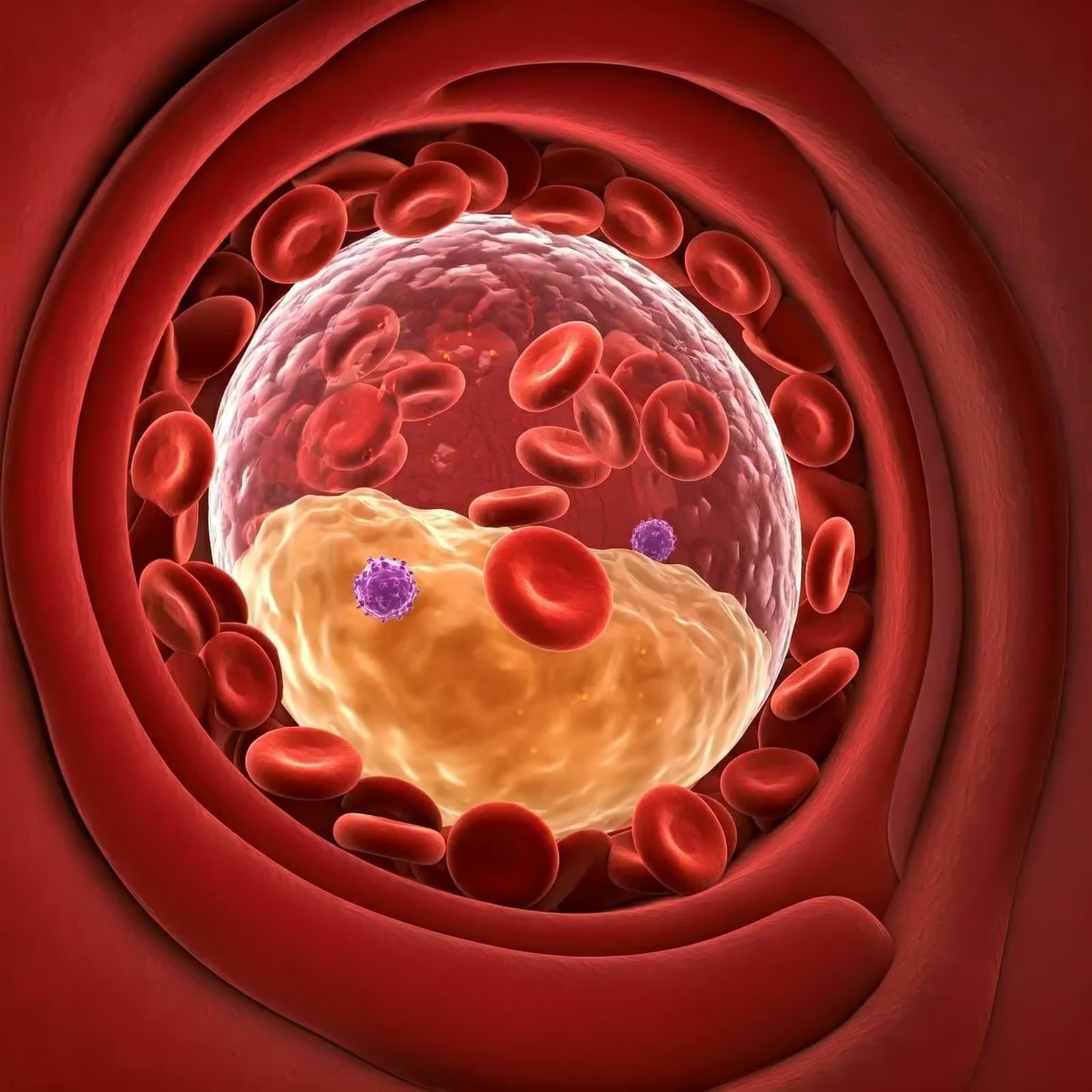
The very act of injecting a filler into the skin, regardless of the technique employed, inevitably causes micro-trauma to the tissues. This trauma initiates the body’s natural inflammatory response, a cascade of biological events designed to repair damage and defend against potential infection. This inflammatory response involves:
- Vasodilation: Blood vessels in the treated area dilate, increasing blood flow to the site. This contributes to redness and warmth.
- Increased Vascular Permeability: The walls of blood vessels become more permeable, allowing fluid and immune cells to leak into the surrounding tissues. This is a primary driver of swelling.
- Immune Cell Recruitment: Immune cells, such as neutrophils and macrophages, migrate to the injection site to clear debris and initiate tissue repair. These cells release inflammatory mediators, further contributing to swelling and discomfort.
The intensity and duration of this inflammatory response can vary depending on several factors. These include the patient’s immune system, the depth and volume of filler injected, and the anatomical location of the treatment.
The Hydrophilic Nature of Hyaluronic Acid Fillers
Hyaluronic acid (HA) fillers are the most widely used type of dermal filler worldwide. HA is a naturally occurring polysaccharide found in the skin and other tissues. Its remarkable ability to bind water molecules gives it its volumising properties. However, this hydrophilic nature also contributes to post-treatment swelling.
When HA filler is injected into the skin, it attracts and holds water, causing the surrounding tissues to expand. This water absorption can persist for several days after the injection, resulting in a gradual increase in swelling. The degree of swelling is influenced by the concentration and cross-linking of the HA filler. Highly cross-linked fillers, which are more robust and longer-lasting, tend to attract less water than less cross-linked fillers.
When HA filler is injected into the skin, it attracts and holds water, causing the surrounding tissues to expand. This water absorption can persist for several days after the injection, resulting in a gradual increase in swelling. The degree of swelling is influenced by the concentration and cross-linking of the HA filler. Highly cross-linked fillers, which are more robust and longer-lasting, tend to attract less water than less cross-linked fillers.
Anatomical Considerations: Areas Prone to Swelling After Filler
Due to their unique tissue characteristics, certain anatomical areas are inherently more prone to swelling after dermal filler injections. These areas include:
- Lips: The lips have a rich vascular supply and a high density of nerve endings, making them particularly sensitive to trauma. The loose connective tissue in the lips also allows fluid to accumulate easily.
- Periorbital Region (Around the Eyes): The skin around the eyes is the thinnest on the body and has a delicate lymphatic drainage system. This makes it susceptible to swelling and bruising.
- Tear Troughs: The tear troughs, the area between the lower eyelid and the cheek, are prone to swelling due to the thin skin, loose connective tissue, and proximity to the lymphatic drainage system.
Individual Patient Factors Influencing Swelling
Individual patient factors can also significantly influence the degree and duration of swelling experienced after dermal filler treatments. These factors include:
- Age: Older individuals may experience more pronounced swelling due to decreased skin elasticity and reduced lymphatic drainage.
- Medications: Certain medications, such as blood thinners and non-steroidal anti-inflammatory drugs (NSAIDS), can increase the risk of bleeding and swelling.
- Medical Conditions: Patients with underlying medical conditions, such as lymphatic disorders or kidney disease, may be more prone to fluid retention and swelling.
- Lifestyle Factors: Smoking, alcohol consumption, and a high-sodium diet can all contribute to increased swelling.
Ultrasound: A Game-Changer in Filler Management
High-frequency ultrasonography (HFUS) has emerged as a valuable tool in the diagnosis and management of dermal filler-related complications, including swelling. Its non-invasive nature, real-time imaging capabilities, and ability to visualise soft tissues make it an ideal modality for assessing filler placement, identifying complications, and guiding treatment.
Ultrasound in Diagnosis: Visualising the Invisible Filler
Ultrasound imaging can provide detailed information about the location, depth, and characteristics of filler material within the tissues. It can help differentiate between filler and other soft tissue structures, such as blood vessels, nerves, and muscle.
Specifically, ultrasound can be used to:
- Confirm Filler Placement: Ultrasound can verify that the filler has been injected into the correct anatomical plane.
- Identify Filler Migration: Ultrasound can detect if the filler has migrated from the intended injection site.
- Detect Early Complications: Ultrasound can identify early signs of complications, such as oedema, haematoma, or inflammatory reactions.
Ultrasound in Management: Guiding Treatment with Precision
Ultrasound-guided techniques can enhance the precision and safety of filler management procedures.
Ultrasound guidance can be used to:
- Localise Filler for Targeted Treatment: Ultrasound can precisely locate filler deposits for targeted treatment with hyaluronidase.
- Guide Hyaluronidase Injections: Ultrasound can guide the injection of hyaluronidase to ensure accurate and efficient dissolution of the filler.
Tear Trough Filler: Unique Challenges and Considerations
The tear trough area presents unique challenges for dermal filler treatments due to the thin skin, delicate lymphatic drainage system, and proximity to the eye. As a result, swelling is a common concern in this area.
Potential Causes of Oedema Following Tear Trough Filler
Oedema in the tear trough area can occur for several reasons, including:
- Filler Hydrophilicity: Certain dermal fillers attract water, resulting in prolonged swelling, particularly in this sensitive area.
- Vascular Irritation: The filler may irritate nearby blood vessels, resulting in increased permeability and fluid retention.
- Lymphatic Disruption: The tear trough region has a delicate lymphatic drainage system, which can become compromised, leading to fluid accumulation.
- Incorrect Placement or Product Choice: Some fillers are too thick for this area or may have been placed too superficially, causing prolonged swelling and irregularities.
- Chronic Inflammation or Biofilm Formation: In rare cases, low-grade inflammation or biofilms (bacterial colonies that form around filler) can contribute to persistent swelling.
Strategies for Minimising Swelling in the Tear Trough
To minimise the risk of swelling in the tear trough area, practitioners should:
- Select Appropriate Filler: Choose a filler specifically designed for the tear trough area with low hydrophilicity and appropriate viscosity.
- Use Conservative Volumes: Inject small volumes of filler to avoid overfilling and excessive pressure on the tissues.
- Employ a Deep Placement Technique: Inject the filler deep to the muscle layer to minimise the risk of lymphatic disruption.
- Avoid Aggressive Injection Techniques: Use a slow and gentle injection technique to minimise trauma to the tissues.
- Consider Cannula Use: Utilise blunt-tipped cannulas to reduce the risk of vascular injury.
Hyaluronidase: The Reversal Agent for HA Fillers
Hyaluronidase is an enzyme that breaks down hyaluronic acid. It is a crucial tool for managing complications associated with HA filler injections, including overcorrection, asymmetry, nodule formation, and vascular compromise.
Mechanism of Action
Hyaluronidase works by hydrolysing the glycosidic bonds in hyaluronic acid, breaking it down into smaller fragments that are then absorbed by the body. Its effects are rapid, with a visible reduction in filler volume occurring within hours of injection.
Indications for Hyaluronidase Use
Hyaluronidase is indicated for:
- Overcorrection: To reduce excessive volume in areas where too much filler has been injected.
- Asymmetry: To correct imbalances in volume between different sides of the face.
- Nodule Formation: To dissolve palpable lumps or bumps that have formed after filler injection.
- Vascular Compromise: To dissolve filler that is compressing or obstructing blood vessels.
- Persistent Swelling: To break down filler contributing to prolonged oedema.
Administration of Hyaluronidase
Hyaluronidase is typically administered via injection directly into the filler deposit. The required dosage of hyaluronidase depends on the volume of filler to be dissolved and the concentration of the hyaluronidase product. It is essential to perform a skin test before hyaluronidase injection to assess for potential allergic reactions.
While generally safe, hyaluronidase can cause some side effects, including:
- Allergic Reactions: Allergic reactions to hyaluronidase are rare but can occur.
- Swelling and Bruising: Swelling and bruising may occur at the injection site.
- Under-correction: In some cases, multiple injections of hyaluronidase may be required to achieve the desired level of filler dissolution.
Conclusion
Dermal filler swelling is a common and multifaceted issue. By understanding the underlying causes and utilising advanced diagnostic tools like ultrasound, practitioners can minimise the risk of swelling and optimise patient outcomes. The use of hyaluronidase represents a crucial element in the safe management of HA filler complications, providing a means to reverse unwanted effects and restore a natural appearance.
As aesthetic medicine continues to evolve, a comprehensive understanding of filler properties, injection techniques, and complication management is essential for ensuring patient safety and satisfaction. The application of dermal filler has improved many lives, but we must approach this treatment with caution to minimise potential complications. The ideal filler treatment is one where the patient is thrilled with the outcome, and the practitioner is confident that they have minimised the risk.
Frequently Asked Questions About Dermal Filler Swelling
1. How long does dermal filler swelling typically last after dermal filler injections?
The duration of swelling after dermal filler injections can vary depending on several factors, including the type of filler used, the area treated, and individual patient characteristics. Generally, patients can expect:
- Initial swelling: Peaks within 24-72 hours post-treatment
- Moderate swelling: May persist for 5-7 days
- Residual swelling: Can last up to 2 weeks, particularly in sensitive areas like the lips or under the eyes
It is essential to note that while visible swelling typically subsides within two weeks, subtle changes in tissue volume may persist for up to a month as the filler settles and integrates with the surrounding tissues.
2. What can I do to reduce dermal filler swelling?
To minimise swelling after dermal filler treatments, consider the following strategies:
- Apply cold compresses: To reduce inflammation, use ice packs or cold compresses intermittently for the first 24 to 48 hours.
- Avoid strenuous exercise: Refrain from intense physical activity for 24 to 48 hours after treatment.
- Stay hydrated: Drink plenty of water to help flush out toxins and reduce swelling.
- Avoid alcohol and salt: Both can contribute to fluid retention and exacerbate swelling.
- Follow aftercare instructions: Adhere to any specific guidelines provided by your practitioner, which may include avoiding makeup or certain skincare products for a specified period.
3. Are certain fillers more likely to cause swelling than others?
While all dermal fillers can potentially cause some degree of swelling, certain characteristics may influence the likelihood and extent of swelling:
- Hyaluronic acid (HA) fillers: Due to their hydrophilic nature, HA fillers may cause more initial swelling as they attract water. However, this swelling is usually temporary.
- Calcium hydroxylapatite fillers (e.g., Radiesse): These may cause less initial swelling than HA fillers but can lead to more prolonged swelling in some cases.
- Poly-L-lactic acid fillers (e.g., Sculptra): These stimulate collagen production and may cause less immediate swelling but can lead to delayed swelling as collagen builds over time.
The concentration and cross-linking of fillers also play a role, with higher concentrations and more cross-linked products potentially leading to more pronounced swelling.
4. When should I be concerned about swelling after dermal filler treatment?
While some swelling is normal, certain signs may indicate a need for medical attention:
- Severe or worsening swelling, especially if it’s asymmetrical
- Swelling accompanied by severe pain, redness, or warmth in the treated area
- Blanching or discolouration of the skin
- Visual disturbances or severe headache (particularly after treatment in the tear trough or temple areas)
- Swelling that persists beyond two weeks without improvement
These symptoms could indicate more serious complications such as infection, vascular occlusion, or allergic reaction. If you experience any of these, contact your practitioner immediately.
5. Can ultrasound help diagnose and manage dermal filler swelling?
Yes, high-frequency ultrasound (HFUS) has become a valuable tool in managing dermal filler complications, including swelling. Here’s how ultrasound can help:
- Diagnosis: HFUS can visualise the precise location and distribution of filler material, helping to differentiate between normal post-treatment swelling and other complications, such as nodules or vascular compromise.
- Treatment planning: Ultrasound can guide targeted treatments, such as precise hyaluronidase injections to dissolve excess filler, by accurately locating filler deposits.
- Monitoring: Ultrasound allows practitioners to track the resolution of swelling and the integration of filler over time, providing objective data on treatment outcomes.
- Vascular assessment: HFUS can evaluate blood flow in the treated area, helping to identify and manage potential vascular complications early.
While not every clinic may offer ultrasound assessment, its use is becoming increasingly common in advanced aesthetic practices, particularly for complex cases or when managing complications.
Key Takeaways
Dermal fillers provide a valuable solution for facial rejuvenation, but it is essential to be aware of the post-treatment care. Patients should be informed about the potential for swelling and what to expect following injections.