Platelet-rich plasma (PRP) therapy has emerged as a transformative tool in dermatology and trichology, leveraging the body’s natural regenerative processes for clinical and aesthetic enhancement. Central to PRP’s efficacy are platelet-derived growth factors (PDGFs), a family of biomolecules that mediate cellular proliferation, angiogenesis, and extracellular matrix (ECM) remodelling. These mechanisms are pivotal in addressing skin ageing and hair loss, which are major concerns for patients worldwide.
This article comprehensively explores Platelet Derived Growth Factors within PRP therapy, focusing on their biological roles, clinical applications, and synergistic interactions with other growth factors. By examining the science underpinning their therapeutic potential, this review aims to deepen understanding and inspire further innovations in regenerative medicine.

Understanding Platelet Derived Growth Factors (PDGFs)
Platelet-derived growth factors are polypeptide molecules stored in the alpha granules of platelets. Upon platelet activation—triggered by vascular injury or therapeutic intervention—PDGFs are released into the extracellular environment. These biomolecules interact with tyrosine kinase receptors on the surface of target cells, initiating intracellular signalling cascades that regulate cellular proliferation, differentiation, migration, and ECM synthesis.
The Key PDGF Isoforms and Their Biological Functions
- PDGF-AA: This isoform primarily supports epithelial cell proliferation, a critical factor in wound healing and the restoration of the epidermal barrier. Its ability to accelerate keratinocyte turnover helps repair damaged or senescent skin cells, enhancing epidermal resilience.
- PDGF-BB: PDGF-BB is extensively studied for its angiogenic properties and its role in dermal fibroblast activation. It stimulates collagen and elastin production, which are essential for maintaining skin firmness and elasticity. Additionally, its contribution to neovascularisation underpins many of the observed benefits in PRP treatments, particularly in enhancing dermal thickness and radiance.
- PDGF-AB: A hybrid isoform, PDGF-AB combines the effects of PDGF-AA and PDGF-BB, exerting broad reparative effects. Its dual functionality bridges epithelial and stromal regeneration, making it integral to comprehensive tissue repair.
- Platelet Derived Growth Factors do not operate in isolation but function within a network of growth factors, including vascular endothelial growth factor (VEGF), transforming growth factor-beta (TGF-β), epidermal growth factor (EGF), and insulin-like growth factor-1 (IGF-1). These interactions amplify therapeutic outcomes by promoting synergistic effects across multiple biological pathways.
Mechanisms of Action in Skin Rejuvenation
Skin ageing is characterised by structural and functional decline, including diminished collagen synthesis, reduced elastin fibre quality, impaired vascularisation, and slower cellular turnover. PDGFs counteract these processes through a multifaceted approach:
1. Collagen Synthesis and ECM Remodelling
PDGF-BB activates dermal fibroblasts, driving the production of collagen and elastin fibres, which are fundamental to the ECM. Enhanced ECM integrity restores skin firmness and elasticity, reducing the appearance of wrinkles and fine lines. By reorganising ECM components, PDGFs also improve dermal resilience and adaptability.
2. Angiogenesis and Nutrient Delivery
The angiogenic properties of PDGFs, particularly PDGF-BB, stimulate the formation of new blood vessels within the dermis. This improved vascularisation facilitates the delivery of oxygen and essential nutrients, revitalising cellular metabolism and promoting a brighter, more vibrant skin tone. Enhanced blood flow also accelerates the clearance of metabolic waste products, further contributing to skin health.
3. Epidermal Cell Turnover
PDGF-AA supports the rapid turnover of keratinocytes, replacing damaged or aged cells with healthier ones. This process improves skin texture, tone, and barrier function, addressing concerns such as roughness and uneven pigmentation. A stronger epidermal barrier also enhances moisture retention and protection against environmental stressors.
Clinical Evidence Supporting Skin Rejuvenation
Several studies validate the role of PRP in skin rejuvenation. Cervelli et al. (2015) demonstrated significant improvements in skin elasticity and dermal thickness following PRP therapy. Similarly, Cho et al. (2020) reported enhancements in hyperpigmentation, texture, and overall appearance in patients with photoaged skin. These findings underscore the efficacy of PDGFs in reversing age-related changes.
Mechanisms of Action in Hair Regeneration
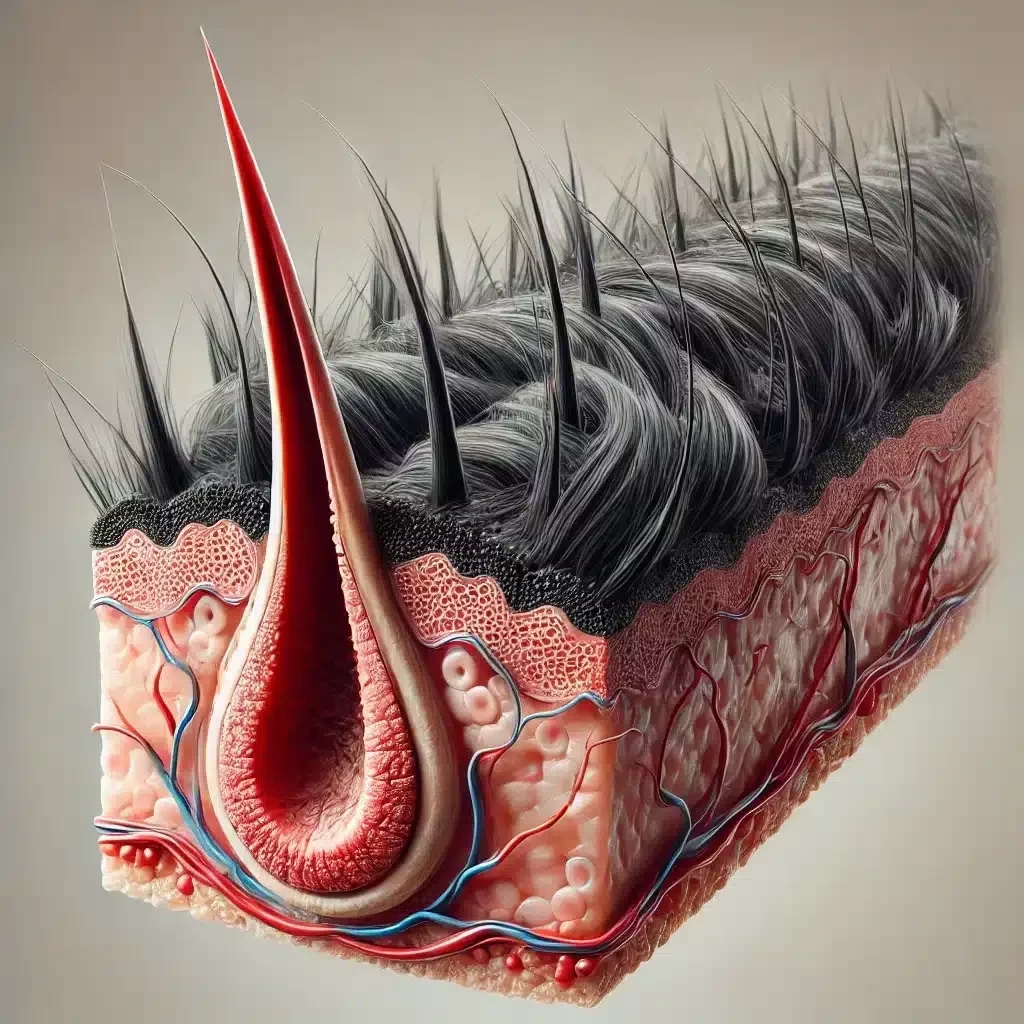
Hair follicles undergo a cyclical growth process comprising three phases: anagen (growth), catagen (regression), and telogen (rest). Disruptions in this cycle result in thinning, shedding, and hair loss. PDGFs play a critical role in restoring follicular health by acting at multiple junctures:
1. Activation of Dermal Papilla Cells (DPCs)
Dermal papilla cells are essential for hair follicle morphogenesis and cycling. PDGF-BB targets these cells to stimulate proliferation and differentiation, facilitating the transition of hair follicles from the resting (telogen) phase to the active growth (anagen) phase. This prolongation of anagen supports robust hair shaft production and improved follicular resilience.
2. Enhanced Follicular Vascularisation
The angiogenic properties of PDGFs improve microcirculation around hair follicles, ensuring a steady supply of oxygen and nutrients. Enhanced vascular support mitigates follicular miniaturisation, a hallmark of androgenetic alopecia, and strengthens hair shafts, reducing breakage.
3. Anti-inflammatory and Antioxidant Effects
Chronic inflammation and oxidative stress destabilise the hair growth cycle, exacerbating hair loss. PDGFs modulate inflammatory pathways and reduce oxidative damage, creating a favourable microenvironment for follicular health.
Clinical Evidence Supporting Hair Restoration
Gentile et al. (2017) conducted a randomised, placebo-controlled trial demonstrating significant increases in hair density and thickness with PRP therapy. A comprehensive review by Alves and Grimalt (2018) further confirmed that PRP consistently improved outcomes in androgenetic alopecia, highlighting the indispensable role of PDGFs in hair restoration.
Synergistic Interactions with Other Growth Factors
The efficacy of Platelet Derived Growth Factors in PRP therapy is enhanced through their interaction with other growth factors:
- Vascular Endothelial Growth Factor (VEGF): VEGF complements PDGF-induced angiogenesis, strengthening vascular support for both skin and hair follicles.
- Transforming Growth Factor-Beta (TGF-β): TGF-β modulates inflammation and encourages ECM production, amplifying PDGF’s effects.
- Insulin-Like Growth Factor-1 (IGF-1): IGF-1 supports cellular proliferation and repair, synergising with PDGFs to enhance dermal and follicular regeneration.
- Epidermal Growth Factor (EGF): EGF promotes keratinocyte proliferation and barrier repair, complementing PDGF’s roles in epidermal turnover and wound healing.
These interactions create a regenerative milieu that maximises therapeutic outcomes.
Clinical Applications and Techniques
Preparation of PRP
PRP is prepared by centrifuging a patient’s blood to isolate platelets, concentrating them to levels several times above baseline. The resulting platelet-rich fraction is rich in Platelet Derived Growth Factors and other growth factors, ensuring a potent therapeutic payload.
Application Techniques
- Skin Rejuvenation: PRP is administered via intradermal injections or combined with microneedling to deliver growth factors directly into the dermis. This dual approach maximises collagen production and enhances skin texture and elasticity.
- Hair Restoration: PRP is injected into the scalp at the level of hair follicles, targeting the dermal papilla cells and surrounding microenvironment. This precise delivery ensures optimal activation of regenerative pathways.
Safety and Tolerability
As an autologous therapy, PRP minimises the risk of adverse reactions. Common side effects, such as mild swelling, redness, and bruising, are temporary and self-limiting. PRP’s favourable safety profile contributes to its growing popularity in aesthetic and clinical dermatology.
Challenges and Future Directions
Despite its promise, PRP therapy faces several challenges:
- Lack of Standardisation: Variability in PRP preparation techniques, growth factor quantification, and administration protocols hinders reproducibility and comparability of clinical outcomes.
- Patient-Dependent Outcomes: Factors such as age, severity of the condition, and individual biological variability can influence treatment efficacy.
Future Research Priorities
- Standardised Protocols: Developing universal guidelines for PRP preparation and application will improve consistency and reliability.
- Combination Therapies: Integrating PRP with stem cells, novel biomaterials, or advanced microneedling devices could enhance therapeutic outcomes.
- Molecular Insights: Investigating the signalling pathways modulated by PDGFs and their interactions with other growth factors may reveal targeted strategies for maximising efficacy.
- Large-Scale Trials: Conducting randomised controlled trials with long-term follow-up will provide robust evidence for the benefits of PRP therapy.
Conclusion
Platelet derived growth factors are pivotal mediators of the reparative and regenerative processes underlying PRP therapy. Platelet Derived Growth Factors improve skin texture, elasticity, and luminosity by stimulating collagen synthesis, angiogenesis, cellular turnover, and anti-inflammatory pathways while promoting robust hair growth and follicular resilience. Their synergistic interactions with other growth factors further enhance the therapeutic impact, solidifying PRP’s status as a cornerstone of regenerative medicine.
As knowledge of Platelet Derived Growth Factors expands, continued research and innovation will refine PRP protocols and integrate emerging technologies, paving the way for more effective and minimally invasive treatments. By harnessing the power of PDGFs, clinicians can offer transformative solutions for addressing skin ageing and hair loss, meeting the growing demand for advanced regenerative therapies.
References
- Alves, R., & Grimalt, R. (2018). A Review of Platelet-Rich Plasma in Androgenetic Alopecia. Dermatol Surg, 44(8), 989-998.
- Cervelli, V., Garcovich, S., Bielli, A., et al. (2015). The Effect of Autologous Platelet-Rich Plasma and Hyaluronic Acid on Skin Elasticity and Dermal Thickness. J Cosmet Dermatol, 14(3), 245-252.
- Cho, J.W., Kim, S.A., & Lee, K.S. (2020). Efficacy of Platelet-Rich Plasma on Skin Rejuvenation in Asians: A Prospective Study. Dermatol Surg, 46(6), 841-849.
- Gentile, P., Garcovich, S., Bielli, A., et al. (2017). The Effect of Platelet-Rich Plasma in Hair Regrowth: A Randomised Placebo-Controlled Trial. Stem Cells Transl Med, 6(4), 1018-1025.
- Marx, R.E. (2004). Platelet-Rich Plasma (PRP): What Is PRP and What Is Not PRP? Implant Dent, 10(4), 225-228.
- Schiavone, G., Raskovic, D., Greco, J., et al. (2014). Platelet-Rich Plasma for Androgenetic Alopecia: A Pilot Study. Dermatol Surg, 40(9), 1010-1019.
- Anitua, E., Sánchez, M., & Orive, G. (2007). Potential of Endogenous Regenerative Technology for Inducing Angiogenesis in Tendon Healing. J Biomed Mater Res Part B, 82B(1), 179-185.
- Kim, D.H., Je, Y.J., Kim, C.D., et al. (2011). Can Platelet-Rich Plasma Be Used for Skin Rejuvenation? Evaluation of Effects on Skin Biomechanics and Histology in Animal Model and Clinical Trials. J Dermatol Sci, 63(2), 80-85
FAQs
1. What are Platelet Derived Growth Factors and how do they support skin and hair regeneration?
Platelet Derived Growth Factors (PDGFs) are naturally occurring proteins found within platelets—blood cells responsible for clotting and healing processes. When applied as part of a regenerative therapy, these growth factors help stimulate the body’s own repair mechanisms. In the context of skin and hair, PDGFs encourage the growth of new cells, improve blood circulation in treated areas, and enhance collagen production. This helps strengthen hair follicles, improve hair density, promote wound healing, and support a more youthful, radiant complexion.
2. How are PDGFs different from other growth factors used in skin and hair treatments?
PDGFs are unique in that they are derived directly from the patient’s own blood, ensuring a highly compatible and biocompatible solution. Unlike synthetic growth factors or laboratory-engineered compounds, Platelet Derived Growth Factors are natural and carry a lower risk of allergic reactions. They are well-studied, versatile, and can be combined with other regenerative approaches, such as Platelet-Rich Plasma (PRP) or microneedling, to enhance overall results.
3. Are PDGF treatments effective for combating hair loss?
Many patients have reported positive outcomes when using PDGF-based therapies for hair loss. By stimulating dormant hair follicles, improving blood flow to the scalp, and encouraging the growth of stronger, thicker strands, Platelet Derived Growth Factors can help slow hair thinning and, in some cases, even restore lost hair. The effectiveness of treatment may vary based on individual factors such as the severity of hair loss, genetics, and lifestyle habits.
4. Can Platelet Derived Growth Factors improve the appearance of ageing skin?
Yes, Platelet Derived Growth Factors can significantly aid in reducing signs of ageing by boosting collagen and elastin production. This leads to firmer, smoother skin with fewer fine lines and wrinkles. Over time, patients may notice improved skin tone, texture, and hydration. While it may not replace more invasive procedures, PDGF therapy often serves as a less intrusive option for rejuvenating dull or ageing skin.
5. How long does it take to see results from PDGF therapy?
Results from PDGF treatments typically become noticeable several weeks to a few months after the procedure, depending on the nature of the concern and the individual’s healing response. For hair regeneration, patients may begin to see improvements in hair texture and density within three to six months. Skin improvements, such as smoother texture or reduced scarring, can appear within a similar timeframe. Multiple sessions may be recommended to achieve optimal, long-lasting results.
6. Are there any side effects or risks associated with PDGF treatments?
Platelet Derived Growth Factors are generally well-tolerated, with minimal side effects due to their natural origin. Mild swelling, redness, or bruising at the injection site may occur but usually resolves within a few days. As PDGFs are derived from the patient’s own blood, the risk of allergic reactions or infections is greatly reduced. However, it is essential to seek treatment from a qualified professional to minimise any potential risks.
7. Is PDGF therapy painful or uncomfortable?
Patients often describe the sensation of PDGF injections as mild discomfort rather than intense pain. Practitioners may apply a topical anaesthetic cream to numb the area before treatment. Most people find that the procedure is manageable, and any lingering tenderness typically subsides within a day or two. Communicating openly with your practitioner can help ensure that comfort measures are taken to minimise discomfort.
8. Can Platelet Derived Growth Factors help treat acne scars or pigmentation issues?
PDGFs have shown promise in improving the appearance of acne scars and other skin irregularities. By stimulating the body’s natural healing response and encouraging the development of healthy new skin cells, PDGF therapy can help even out skin texture and reduce the visibility of scars. Results may vary, and multiple sessions could be necessary to achieve optimal improvement.
9. How often should PDGF treatments be performed for best results?
Treatment frequency depends on the individual’s specific needs, goals, and response to therapy. Many practitioners recommend an initial series of treatments—often three to four sessions spaced a few weeks apart—followed by maintenance sessions every six to twelve months. Your practitioner can create a customised schedule based on your progress and the desired outcome.