Lip enhancement using dermal fillers has surged in popularity, offering individuals fuller and more defined lips. However, the procedure is not without risks, particularly vascular occlusion stemming from inadvertent injection into or compression of the superior and inferior labial arteries. This article explores the use of ultrasound before filler placement to enhance safety, focusing on critical anatomy, potential risks, injection techniques, and various lip augmentation styles.
Understanding Lip Anatomy: Superior and Inferior Labial Arteries
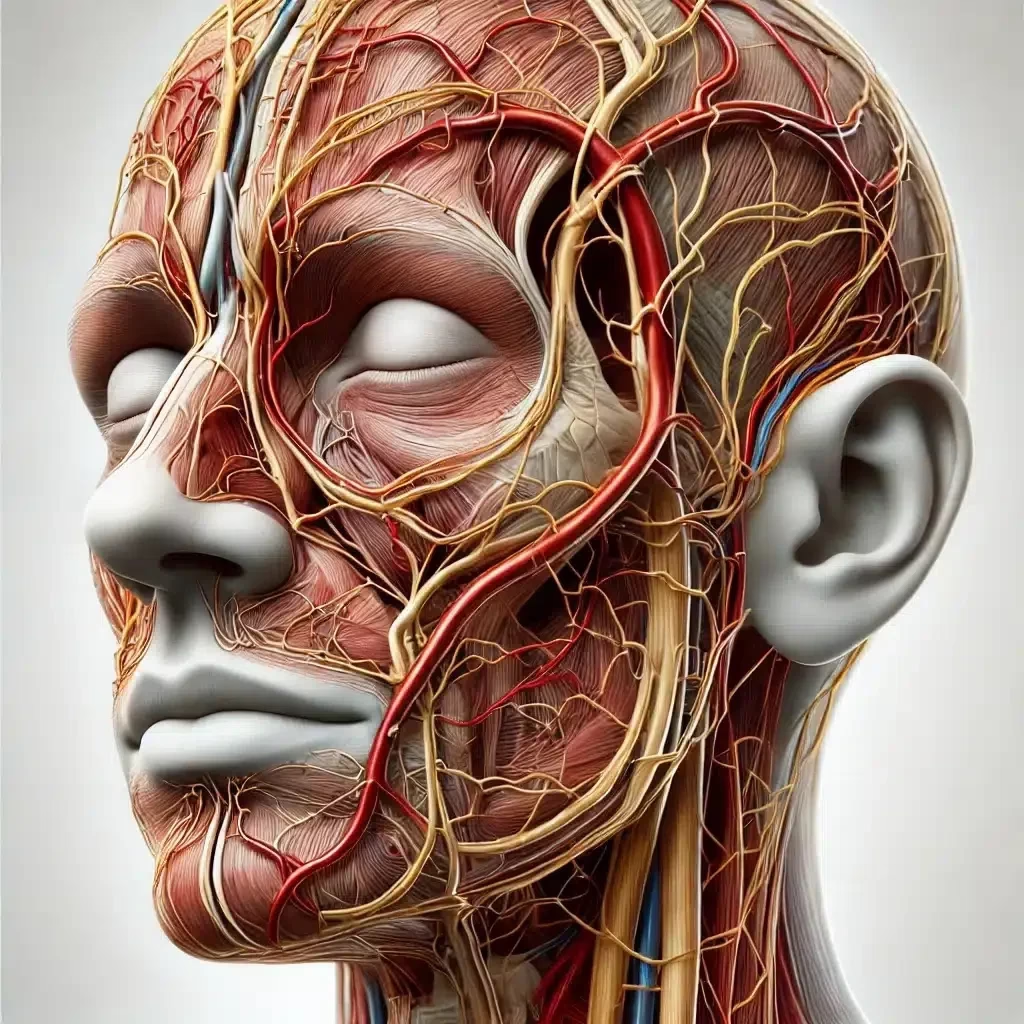
The superior and inferior labial arteries are vital blood vessels supplying the upper and lower lips. Branching from the facial artery, they run horizontally within the lips but can vary in exact location and depth among individuals (DeLorenzi, 2017). Accurate knowledge of their typical pathways is crucial to minimise the risk of vascular complications during filler injections.

Detailed Anatomy of the Labial Arteries: Depth and Location
Understanding the precise depth and location of the labial arteries is essential for safe lip augmentation procedures.
- Superior Labial Artery (SLA):
- Origin and Course: The SLA branches from the facial artery near the angle of the mouth and travels medially along the upper lip.
- Depth: Studies indicate that the SLA is typically located 3 to 5 mm beneath the skin surface but can range from 1.1 mm to 6.9 mm due to individual anatomical differences (Cotofana et al., 2019).
- Location: The artery often runs within the submucosal layer or the orbicularis oris muscle, approximately 6 to 9 mm above the vermillion border. It may have a tortuous path with multiple branches supplying the mucosa, muscle, and skin of the upper lip.
- Inferior Labial Artery (ILA):
- Origin and Course: The ILA also branches from the facial artery near the corner of the mouth and courses medially along the lower lip.
- Depth: The ILA is usually situated 4 to 6 mm beneath the skin but can vary between 1.2 mm and 7.0 mm (Koh et al., 2018).
- Location: It typically lies within the submucosal layer or orbicularis oris muscle, about 5 to 8 mm below the vermillion border. Like the SLA, the ILA may have a variable path with several branches.
- Anatomical Variations:
- Depth Variability: The depth of labial arteries can vary due to age, gender, ethnicity, and previous procedures.
- Branches and Anastomoses: Both arteries may have multiple branches and connections with other vessels, increasing the complexity of the vascular network in the lips.
- Implications for Injections: Due to this variability, it’s challenging to predict the exact location of the arteries without imaging assistance.
- Importance of Ultrasound:
- Visualisation: Ultrasound imaging can identify the precise location and depth of the labial arteries in each patient.
- Injection Planning: By mapping these arteries, practitioners can plan injection sites that avoid vascular structures, reducing the risk of intravascular injection.
- Dynamic Assessment: Ultrasound allows real-time assessment during injections, enhancing safety.
Understanding these details helps practitioners choose appropriate injection depths and techniques, such as staying superficial to the artery (less than 3 mm depth) or deep to it (more than 6 mm depth), depending on the area and desired outcome. However, given the anatomical variability, reliance solely on standard measurements without imaging may not suffice for safe practice.
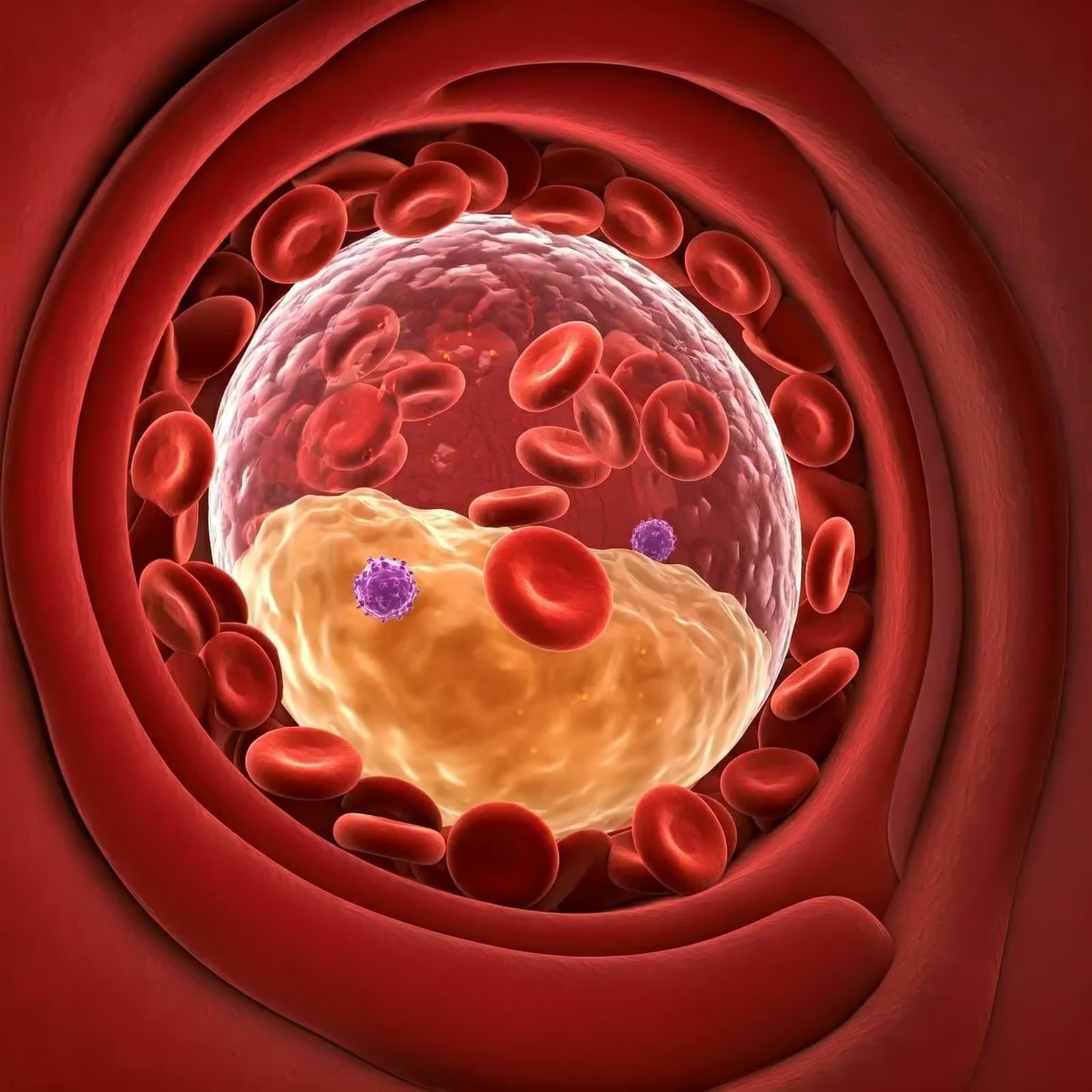
Risks of Dermal Filler Placement: Vascular Occlusion
A significant risk associated with lip filler injections is vascular occlusion. This occurs when filler material inadvertently enters a blood vessel, leading to blockage, tissue ischaemia, and potential necrosis (Heydenrych & Kapoor, 2018). Symptoms may include pain, blanching, and discolouration. Immediate recognition and intervention are essential to prevent long-term tissue damage.
The Role of Ultrasound in Enhancing Safety
Pre-procedural ultrasound allows practitioners to map out the vascular anatomy of the lips, identifying the precise location of the labial arteries (Wortsman et al., 2020). By visualising these arteries, clinicians can plan injection sites strategically to minimise the risk of vascular occlusion. Ultrasound guidance can also assist in real-time monitoring during the injection process.
Limitations of Ultrasound
Despite its advantages, ultrasound has limitations in lip enhancement procedures:
- Technical Challenges: The lips’ small and curved anatomy can make ultrasound imaging difficult (Roberts et al., 2019).
- Operator Dependence: Accurate imaging requires significant skill and experience.
- Time Constraints: Ultrasound mapping requires additional time, which may not be practical in all clinical settings.
- Equipment Costs: High-quality ultrasound devices represent a financial investment.
Impact of Scar Tissue and Arterial Fixation
Previous lip procedures, trauma, or infections can lead to scar tissue formation, potentially fixing the arteries in place rather than allowing them to be mobile (Kim et al., 2016). Fixed arteries are at a higher risk of being punctured during injection. Ultrasound can help identify areas of scar tissue, enabling practitioners to adjust injection techniques accordingly.
Needles vs Cannulas: A Safety Comparison
The choice between needles and cannulas impacts the safety profile of lip filler injections:
- Needles:
- Advantages: Greater precision and ease of insertion in tight spaces.
- Disadvantages: Sharp tip increases the risk of penetrating blood vessels, leading to vascular occlusion.
- Cannulas:
- Advantages: Blunt tip reduces the risk of vascular injury by pushing vessels aside.
- Disadvantages: Less manoeuvrable in the confined lip area, potential for inadequate filler placement.
Studies suggest that using cannulas may reduce the incidence of vascular complications (Sundaram et al., 2015), but the practitioner’s expertise and the specific clinical scenario should guide the choice of instrument.
Popular Lip Augmentation Techniques and Associated Risks
In addition to the ‘Russian Lips’ technique, which involves injecting filler vertically to create a heart-shaped, voluminous appearance, several other lip augmentation methods are popular among practitioners and patients. Each technique offers unique aesthetic outcomes and varies in injection approach, filler placement, and overall lip appearance. Understanding these techniques and their associated risks is essential for safe practice.
1. Classic Lip Augmentation
- Description: Enhances the natural shape and volume of the lips proportionally.
- Method: Even distribution of filler along the vermillion border and body of the lips using linear threading or serial puncture techniques.
- Risks: General risks of filler injections apply, including vascular occlusion, if not performed carefully.
2. Paris Lip Technique
- Description: Creates a well-defined lip border and accentuates the Cupid’s bow.
- Method: Micro-droplets of filler are placed along the vermillion border.
- Risks: Over-emphasis may lead to an unnatural appearance; careful placement is necessary to avoid vascular structures.
3. Keyhole Lip Technique
- Description: Produces a small gap or ‘keyhole’ effect in the centre of the lips when closed.
- Method: Filler is strategically injected to enhance the central tubercles of the upper and lower lips.
- Risks: Requires precision to avoid asymmetry and vascular complications.
4. Tenting Technique
- Description: Increases the vertical height of the lips without significant forward projection.
- Method: Vertical injections perpendicular to the lip border.
- Risks: Vertical injections may come closer to labial arteries, increasing the risk of vascular injury.
5. Heart-Shaped Lips
- Description: Creates a heart-like appearance by emphasising the Cupid’s bow and central lower lip.
- Method: Targeted injections in central areas of the lips.
- Risks: Overfilling can lead to an unnatural appearance; care is needed to avoid vascular occlusion.
6. Linear Threading Technique
- Description: Enhances shape and volume using linear filler placement.
- Method: Filler injected in linear threads along lip contours.
- Risks: Risk of traversing vascular structures if not carefully planned.
7. Microbolus Technique
- Description: Involves depositing small amounts of filler at multiple points.
- Method: Serial puncture injections delivering micro boluses.
- Risks: Increased number of injections can raise the risk of bruising and vascular injury.
8. Pillar Technique
- Description: Creates vertical pillars of filler to add structure and volume.
- Method: Vertical linear injections from the mucosal side of the lip.
- Risks: Similar to tenting, vertical injections may increase vascular injury risk.
9. Border Enhancement (Vermillion Border Definition)
- Description: Enhances the outline of the lips without significant volume addition.
- Method: Filler injected along the vermillion border.
- Risks: Superficial placement near vascular networks requires precision to avoid complications.
Each technique should be chosen based on the patient’s anatomical features, desired outcome, and safety considerations. Practitioners must have a thorough understanding of lip anatomy and tailor the approach to individual needs. Ultrasound imaging can assist in planning and executing these techniques safely by mapping out critical anatomical structures.
Risks Associated with Trends: The ‘Russian Lips’ Technique and Others
Trends like the ‘Russian Lips’ technique and other specialised methods may increase risks due to:
- Proximity to Labial Arteries: Certain techniques involve injections closer to arterial pathways.
- Increased Volume or Height: Techniques aiming for significant augmentation may raise the likelihood of vascular compression.
- Technique Sensitivity: Many specialised methods require high skill to avoid complications.
Practitioners should exercise caution and ensure thorough anatomical knowledge when performing such trend-driven procedures (Liew et al., 2020).
Injection Techniques for Lip Filler Placement
Various injection techniques can be employed, each with its considerations:
- Linear Threads: Injecting filler along the lip’s length to enhance shape and volume.
- Pros: Even distribution, natural look.
- Cons: Risk of traversing vascular structures.
- Boluses: Depositing small amounts of filler at specific points.
- Pros: Allows targeted augmentation.
- Cons: Higher risk of lumpiness and vascular occlusion if placed improperly.
- Fanning and Cross-Hatching: Multiple injections creating a mesh-like filler distribution.
- Pros: Smooths out irregularities.
- Cons: Increases the number of entry points, potentially raising complication risks.
Selecting the appropriate technique depends on the patient’s anatomy, desired outcome, and the practitioner’s experience. Ultrasound can help by mapping out critical anatomical structures, aiding in choosing and executing the safest technique.
Conclusion – Ultrasound Guided Lip FIller Injections
Ultrasound is a valuable tool in enhancing the safety of lip filler procedures by providing real-time visualisation of critical vascular structures. While limitations exist, its use can significantly reduce the risk of vascular occlusion when combined with thorough anatomical knowledge and careful injection techniques. Understanding the implications of scar tissue, instrument choice, various lip augmentation techniques, and trending procedures like the ‘Russian Lips’ method further contributes to safer and more effective lip enhancement outcomes.
References
- Cotofana, S., et al. (2019). Distribution pattern of the superior and inferior labial arteries: impact for safe augmentation procedures. Plastic and Reconstructive Surgery, 143(5), 1283–1292.
- DeLorenzi, C. (2017). Complications of injectable fillers, part 1. Aesthetic Surgery Journal, 37(7), 887–899.
- Heydenrych, I., & Kapoor, K. M. (2018). The wrinkle and the scar: preventing and managing dermal filler complications. Journal of Cutaneous and Aesthetic Surgery, 11(1), 30–38.
- Kim, J. E., et al. (2016). Vascular complications of hyaluronic acid fillers and the role of hyaluronidase in management. Journal of Cosmetic and Laser Therapy, 18(4), 256–261.
- Koh, K. S., et al. (2018). Location of the superior and inferior labial arteries: implication for lip augmentation using injectable fillers. Dermatologic Surgery, 44(5), 684–689.
- Liew, S., et al. (2020). Facial injectables in aesthetic medicine: facial assessment and injection techniques for botulinum toxin and fillers—an anatomical viewpoint. Journal of Cutaneous and Aesthetic Surgery, 13(2), 74–87.
- Pessa, J. E., et al. (2018). The anatomical basis for tissue repositioning of the nasolabial fold. Plastic and Reconstructive Surgery, 141(5), 1084–1091.
- Roberts, S. A., et al. (2019). High-resolution ultrasound for the investigation of dermal fillers. Clinical and Experimental Dermatology, 44(3), 314–317.
- Sundaram, H., et al. (2015). Blunt-tipped microcannula technique for soft tissue filler injection: international consensus recommendations. Plastic and Reconstructive Surgery, 136(1S), 28S–35S.
- Wortsman, X., et al. (2020). Ultrasound in facial fillers evaluation and complications. Journal of Ultrasound in Medicine, 39(7), 1331–1339.